Systematic quantification and evaluation will shape surgical, transcatheter treatment of valve dysfunction
As the population ages, the clinical impact of mitral annular calcification (MAC) looms large due to its various pathophysiologic manifestations. Despite this impact, there is no universally accepted grading system for MAC severity.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
To fill this gap, a Cleveland Clinic team led by cardiovascular imaging specialist Bo Xu, MD, recently developed a novel multi-parametric grading system for MAC based on qualitative and quantitative measurements. The grading system has been published in EHJ: Cardiovascular Imaging.
“Mitral annular calcification is an underappreciated entity that can contribute to significant cardiac risk,” Dr. Xu says. “It deserves heightened attention.”
The condition has occupied Dr. Xu’s interest for several years. While reading thousands of CT scans and echocardiograms, he noticed MAC becoming increasingly prevalent, particularly in older patients.
“MAC is a complex, multifaceted entity, but it has not been well researched,” he says. “There is no good system for describing it or assessing its severity, so it is too often underappreciated or simply ignored. However, MAC will be present whether we pay attention to it or not, so we should be more aware of MAC as an entity.”
In 2016, a system for classifying MAC was proposed that based classification on the qualitative extent of calcification derived from parasternal short-axis echocardiographic imaging.
Dr. Xu felt the process of evaluating and grading MAC needed to be supplemented with additional information that could be obtained only through additional imaging techniques. Over time, he examined the potential value of several imaging modalities. Ultimately, he found a combination of echocardiography and cardiac CT to be most valuable for a systematic and quantitative approach to evaluating MAC severity (see Figure below).
Advertisement
Cardiac CT is critical due to its superior ability to define and quantify calcification. “Quantification of mitral annual calcification with the Agatston method is a key strength of CT,” Dr. Xu explains.
CT also serves to quantify the extent of calcification and to assess for special features, including extent of intrusion into the left ventricular outflow tract and infiltration of calcification into the myocardium.
These imaging features were then used to form an overall MAC grade, ranging from 1 to 4, with 4 being the most severe. This approach potentially allows for a reproducible quantitative MAC grading system that can be used to improve preoperative planning, patient selection and risk stratification.
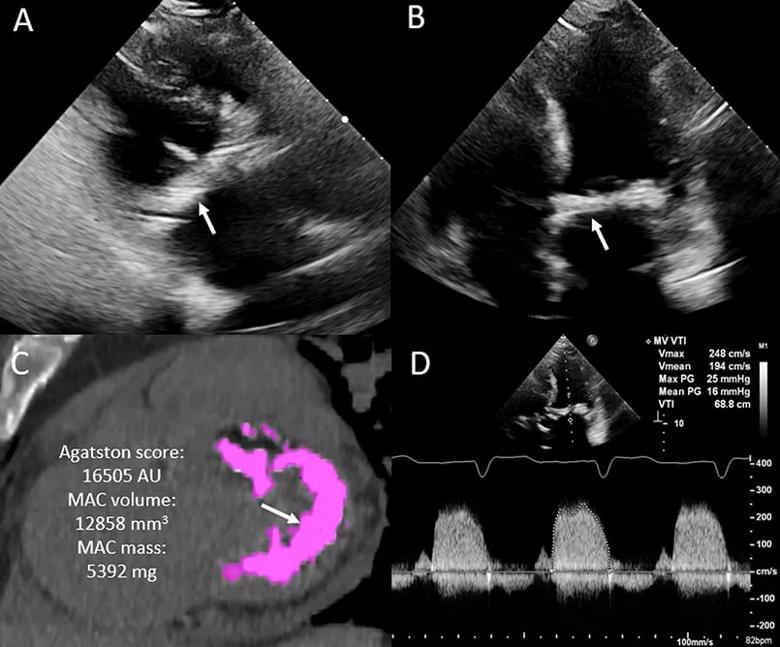
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/baaeabfc-075c-4e30-852c-386d0fe2307a/21-HVI-2396964-Inset-805x668-1_jpg)
Figure. Severe mitral stenosis due to mitral annular calcification. (A) Transthoracic echocardiogram (parasternal long-axis view) showing significant mitral annular calcification (MAC) (arrow). (B) Transthoracic echocardiogram (apical four-chamber view) showing significant MAC (arrow). (C) Cardiac CT showing circumferential MAC (arrow), with significantly elevated Agatston score, MAC volume and mass. (D) Continuous-wave Doppler through the mitral valve demonstrating elevated gradients (peak/mean: 25/16 mmHg at 82 BPM), consistent with significant calcific mitral stenosis.
MAC can be a benign, incidental finding, but some patients develop associated mitral valve dysfunction, arrhythmias and (in rare cases) endocarditis. Symptomatic patients with severe MAC and severe mitral regurgitation or stenosis require definitive treatment, which often means surgery at an experienced center. One reason for understanding MAC severity is to provide a framework for understanding how these patients should be risk stratified and treated.
Advertisement
“Reproducible MAC quantification has potential prognostic significance, and it may be important in guiding management, including transcatheter and surgical mitral valve interventions,” says Dr. Xu.
He and his colleagues are now studying all MAC patients treated surgically at Cleveland Clinic to validate the grading system. “It will be a solid body of evidence that should be helpful for clinical practice,” he says.
Other clinicians have been quick to recognize that the grading system fills an important knowledge gap.
“In their new paper, Dr. Xu and co-authors review a clinically relevant but underappreciated topic, highlight the importance of multimodality imaging in the assessment of mitral annular calcification and propose a much-needed classification system for its severity,” says Serge Harb, MD, a Cleveland Clinic cardiologist who was not involved in this project. He has developed expertise in displaying MAC on CT studies and assisting surgeons and interventionalists in formulating specific treatment plans.
Cardiothoracic surgeon Shinya Unai, MD, a co-author of the new paper, notes that he and his colleagues are now able to operate safely on patients with MAC who would have been deemed too high-risk even a few years ago. He looks forward to the enhanced guidance that the MAC grading system will provide in practice.
“To grade mitral annular calcification, advanced imaging techniques and CT reconstruction are necessary,” Dr. Unai explains. “During that process, we look closely at the distribution of calcification, identify high-risk features that could lead to a poor outcome, and perform risk assessment for surgical planning. As a result of these applications of advanced imaging techniques, surgical interventions to address mitral annular calcification have become much safer.”
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more