Posterior endoscopic graft suturing may reduce costs and risks associated with postoperative intubation or tracheostomy placement in children

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Endoscopic posterior cricoid split with costal cartilage grafting (EPCSCG) is a minimally invasive surgical option for young patients with subglottic stenosis, posterior glottis stenosis and bilateral vocal fold immobility. This approach has several advantages compared to an open approach; however, there is risk that the graft will become dislodged and obstruct the airway. In the past, this risk has been mitigated by stenting, either with a prolonged period of endotracheal intubation or placement of a stent above a tracheostomy.
We propose an endoscopic suturing technique for securing the graft in EPCSCG. We believe this technique, which we have successfully performed twice, further decreases the duration of postoperative intubation and may result in shorter ICU stays.
We approach EPCSCG as described in the literature; however, we suture the graft in place. To achieve this, we created a horizontal mattress by passing a double needle 5.0 PDS suture through the posterior portion of the larynx above the esophageal inlet. We harvest a costal cartilage graft, carving it with anterior flanges and slightly tapering the inferior aspect before coring small holes through the cartilage with a 22 gauge needle.
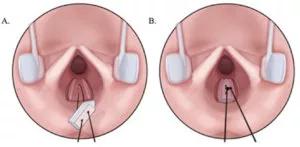
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/71cf41fd-33b0-420c-a1a3-c153ddd82d98/placing-the-graft-300x147_jpg)
With holes slightly larger than the suture, the graft is sutured in place using the novel endoscopic suturing technique.
We then pass the previously placed PDS suture through the graft at the suture sites, parachuting the graft into the cricoid split. After locking the graft in place, we tie the free edges of the sutures into a square not with a single throw.
Advertisement
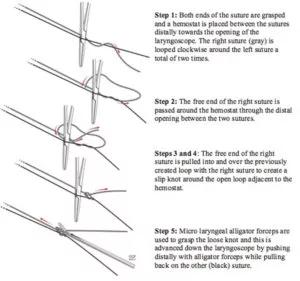
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/dd729427-c959-4222-af37-d53b96af3e9b/Suture-technique-300x281_jpg)
Endoscopic suturing technique for graft securement.
Thus far, we have performed this procedure twice at Cleveland Clinic’s Pediatric Center for Airway, Voice and Swallowing Disorders. Our first patient (P1) was a 3-year-old with a history of prolonged intubation following surgical repair for Tetralogy of Fallot with absent pulmonary valve as an infant. On exam, the patient had inspiratory stridor. We conducted in-office flexible laryngoscopy, which revealed hypomobile vocal cords in paramedical position with limited bilateral abduction. Operating room airway evaluation revealed airway obstruction that included posterior glottis stenosis, a subglottic cyst, a small anterior glottis web and moderate tracheomalacia.
In P1, we placed the EPCSCG with sutured graft without tracheostomy. The patient was extubated in the operating room on postoperative day (POD) three, and direct laryngoscopy revealed a healing graft secured by intact suture. There were no postoperative complications. P1 was discharged home on POD six.
By the one-month follow-up visit, P1’s stridor had resolved completely, voice was improved and P1 was able to tolerate a regular diet. At nine months postop, we evaluated the airway in the operating room and found no evidence of stenosis and a well-healed cartilage graft.
Our second patient (P2) was a toddler with bilateral vocal cold paresis of unclear etiology who had been tracheostomy dependent since two to three weeks of age. We discovered and removed a large vallecular cyst during airway evaluation. Postoperative flexible laryngoscopy revealed vocal folds in median position, but we found it difficult to access their mobility. We reduced the size of the tracheostomy from 3.5 to 3.0 uncuffed flexible Bivona. Two months later, we were better able to access the vocal cords, and found them to be immobile, in the median position bilaterally.
Advertisement
We performed EPCSCG, securing the graft using our endoscopic suturing technique, but left the tracheostomy in place. No stenting was required. P2 also had an uncomplicated postoperative stay and was discharged on POD four. At two weeks postop, we performed a scheduled airway evaluation that revealed a healing graft and improved glottis airway. We have scheduled a repeat airway evaluation, during which we hope to trial capping and decannulation.
This sutured graft technique has been described in only five studies, which recommend that this procedure be conducted with a tracheostomy in place or with a prolonged period of postoperative intubation to reduce the risk of graft extrusion and potential airway obstruction. We note that the majority of patients in these studies had previously placed tracheostomies at the time of EPCSCG. There have only been six cases of EPCSCG reported without tracheostomy.
To our knowledge, this is the first report of endoscopic placement of a sutured posterior graft. Although we acknowledge the need for a larger series to confirm the safety and efficacy of endoscopic posterior graft suturing without the need for prolonged intubation or stent placement above a tracheostomy, we believe this technique may further decrease the required hospital stay and reduce the risks and costs related to tracheostomy placement in a pediatric population.
Note: Medical art reused with permission from Elsevier; originally published in: Shah J, Ciolek P, Hopkins B. Novel endoscopic suturing technique to mitigate risk of graft extrusion in
endoscopic posterior cricoid split and costal cartilage grafting: A case report. Int J Pediat Otolaryngol. 2018;(109):164-167. doi: 10.1016/j.ijporl.2018.04.012
Advertisement
Advertisement

Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor

Case study illustrates the potential of a dual-subspecialist approach

Evidence-based recommendations for balancing cancer control with quality of life

Study shows no negative impact for individuals with better contralateral ear performance

HNS device offers new solution for those struggling with CPAP

Patient with cerebral palsy undergoes life-saving tumor resection

Specialists are increasingly relying on otolaryngologists for evaluation and treatment of the complex condition

Detailed surgical process uncovers extensive middle ear damage causing severe pain and pressure.