Delaying treatment of ectopic pregnancy is dangerous
In late November 2019, the Ohio State House of Representatives introduced a bill that addresses pregnancy and termination, and would require physicians to “take all possible steps to preserve the life of the unborn child, while preserving the life of the woman.” The bill, HB 413, states that these steps “include, if applicable, attempting to reimplant an ectopic pregnancy into the woman’s uterus.”
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Even before this bill, it was natural for a woman to ask if there was any way to save a pregnancy. There’s always been that question. If there’s any way for us to save a pregnancy, we are going to do it – but reimplanting an ectopic pregnancy is simply not plausible,” states Salena Zanotti, MD, an Ob/Gyn with the Cleveland Clinic Ob/Gyn & Women’s Health Institute.
Although the treatment of ectopic pregnancy has evolved over the last few decades, physicians agree that reimplantation remains a medical impossibility. In a recent article from the European Journal of Obstetrics, Gynecology and Reproductive Biology, researchers reviewed randomized clinical trials from the past 30 years that evaluated different interventions for the condition. Not one discussed reimplantation of an ectopic pregnancy. According to Drs. Rao and Zanotti, there’s good reason for this.
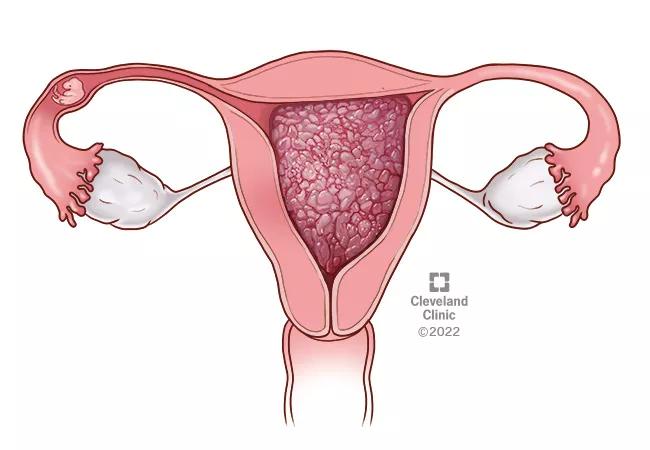
An ectopic pregnancy occurs when a fertilized ovum implants outside the uterus, most commonly in the fallopian tube. Ectopic pregnancies occur in less than 2% of all pregnancies, and are considered dangerous for women because, as the pregnancy grows, it can rupture and cause life-threatening internal bleeding. “These pregnancies can never become normal, viable pregnancies,” Dr. Zanotti adds.
Historically, these extrauterine pregnancies were treated with abdominal surgery (i.e., either salpingostomy or salpingectomy). “We then converted those procedures to laparoscopic procedures to make them less invasive. In the mid-1990s, we started treating appropriate candidates with methotrexate in order to avoid the operating room altogether. But compliance is key for medical therapy, as patients need to follow a series of rigorous standards for follow-up,” explains Ken Rao, MD, Director of Obstetrics at Cleveland Clinic Hillcrest Hospital.
Advertisement
“These are pregnancies that you need to disrupt for the mother’s safety. And once you’ve disrupted it, there is no way of implanting it. I don’t think anyone’s ever even considered looking at doing this because it makes no sense from a scientific standpoint,” Dr. Zanotti says.
For a pregnancy to progress, two things must happen in coordination: the embryo has to leave the fallopian tube and implant in the uterus, which must be able to receive it, according to Dr. Rao. If you disrupt it from the implantation site, the embryo loses its blood supply. Even if you were able to reestablish implantation within the uterus, the uterine lining would have lost its ability to support the pregnancy.
“This is why there are no studies,” Dr. Rao continues.
Receiving a diagnosis of ectopic pregnancy is already tumultuous for women. Ob/Gyns like Drs. Rao and Zanotti are concerned that by allowing language like this in a bill, women may second guess the advice of their physicians. “Delaying treatment of ectopic pregnancy can be catastrophic,” says Dr. Zanotti. “Furthermore, the language in the bill may compound feelings of guilt and shame in women.”
“When we confirm ectopic pregnancy through ultrasound and labs, most women are devastated to learn that there is no way for the pregnancy to be viable. It’s not a casual conversation,” Dr. Rao says.
Advertisement
Advertisement

Uterine transposition cleared the field for radiation therapy

ACOG-informed guidance considers mothers and babies

Prolapse surgery need not automatically mean hysterectomy

Artesunate ointment shows promise as a non-surgical alternative

New guidelines update recommendations

Two blood tests improve risk in assessment after ovarian ultrasound

Recent research underscores association between BV and sexual activity

Psychological care can be a crucial component of medical treatment