Studies continue to indicate effectiveness and safety
Losartan, an angiotensin-converting enzyme (ACE) II receptor antagonist, is one of the most commonly used oral medications for hypertension. It’s also known to inhibit transforming growth factor (TGF) beta signaling, a process behind the development of corneal myofibroblasts, the main cause of severe, persistent corneal scarring after infection, injury or refractive surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Noting the TGF beta connection, researchers led by refractive surgeon Steven E. Wilson, MD, Director of Corneal Research at Cleveland Clinic Cole Eye Institute, have developed topical losartan for treating corneal scarring caused by myofibroblasts.
The outcomes of studies on topical losartan over the past two years have been so promising, that losartan is now being used successfully off-label around the world.
“The clinical results reported for this new treatment have been spectacular in all kinds of corneal scars, with zero side effects or complications reported to date,” Dr. Wilson says.
Administered as a drop in the eye six times per day, “there’s no stinging or irritation whatsoever, so patients are much more likely to stay with the regimen,” he says.
The research team’s most recent study, published this year in Cornea, examined the effect of vehicle versus topical losartan in models of deep corneal laceration. The researchers simulated lacerations with a single 0.35-mm deep incision in the center of the corneas and treated them with either 50 μL of topical 0.8 mg/mL losartan or 50 μL of balanced salt solution six times per day for one month.
The study found that losartan significantly decreased myofibroblasts surrounding the laceration but did not prevent the laceration from closing.
“It’s thought that myofibroblasts’ purpose is to hold tissue together, but that wasn’t the case in this study,” Dr. Wilson says. “It’s probably not the myofibroblasts that are closing these lacerations, but rather corneal fibroblasts, which aren’t significantly affected by losartan.”
Advertisement
Dr. Wilson believes these results indicate that losartan will be useful in corneas that either have an incision that becomes more scarred than expected or in patients who develop scarring after a laceration.
Another recent study by Dr. Wilson’s team (publication pending) used model corneas to investigate the maximum dose of topical losartan for human corneas. The study found that the highest concentration used clinically should be 0.8 mg/mL.
“Because our previous studies have shown that lower doses of 0.2 mg/mL worked to clear myofibroblasts, and because this study found some evidence of epithelial toxicity, our recommendation is that in patients with an epithelial defect, only 0.2 mg/mL six times a day be used until the epithelium heals. After that, they can increase to 0.8 mg/mL,” Dr. Wilson says.
Dr. Wilson’s lab has been funded for more than 30 years by the National Institutes of Health or Department of Defense to examine corneal wound healing. The research team has been conducting studies on losartan for the past five years.
In their first study, the team successfully used topical losartan to clear posterior corneal scars after descemetorhexis, the surgical removal of a patch of the endothelium and Descemet’s membrane. This study showed that topical losartan can pass through the intact epithelium and epithelial basement membrane.
In another study, the researchers found that a combination of topical losartan and corticosteroids best reduced corneal scarring after alkali burns. Likely, this combination will be the best treatment for disorders with severe inflammation, such as alkali burns and severe infections (along with antibiotic, antiviral or anti-acanthamoebic medications), notes Dr. Wilson.
Advertisement
Studying anterior scarring from myofibroblast generation after high photorefractive keratectomy (PRK) in animal models, a third investigation found that losartan was effective in decreasing scarring after PRK without the use of mitomycin C. While Dr. Wilson continues to use topical mitomycin C at the time of PRK, he believes topical losartan will be beneficial for treating breakthrough haze that occurs despite mitomycin C.
A fourth study evaluated the effect of topical losartan on surface blast-simulating irregular phototherapeutic keratectomy (PTK) in animal models, similar to what members of the military could experience in combat.
“The losartan did decrease myofibroblast generation, but it didn’t decrease the scarring or the opacity in the cornea because the irregular surface itself causes opacity,” says Dr. Wilson. “This shows that in those corneas with a very irregular surface, you first need to do a surgery such as PTK to decrease the surface irregularity and then treat with losartan to be most effective.”
Losartan does not affect corneal scars that are not caused by myofibroblasts, such as early haze after PRK, which is caused by corneal fibroblasts.
“You don’t need to treat this anyway because it goes away on its own,” Dr. Wilson says.
Losartan also is unnecessary for treating the transient anterior haze that develops after normal corneal cross-linking, also caused by corneal fibroblasts. However, a soon-to-be-published case study by another research group involved using topical losartan to successfully treat a patient with a rare case of vision-limiting scarring after cross-linking.
Advertisement
“Basically, we anticipate that any scarring caused by myofibroblasts could be effectively treated with topical losartan, and that’s 99% of the scars ophthalmologists see,” Dr. Wilson says.
According to Dr. Wilson, one of his former research fellows now practicing in Brazil is currently using losartan to treat a patient with a three-year-old herpes zoster scar that had markedly decreased her vision. The patient is still undergoing treatment, but within four months, her visual acuity has improved to 20/30.
This inspired Dr. Wilson and his team to perform another study (publication pending) to investigate therapeutic use of losartan.
“All the animal model studies we had done so far were prophylactic, so we did a study where we let alkali burns in corneas heal for a month and develop fibrosis, then started losartan, and it still worked perfectly,” Dr. Wilson says. “This confirmed what we’d found in humans — that losartan can be used either prophylactically to prevent scarring or therapeutically on a scar that has been there for years.”
Dr. Wilson encourages physicians to consider using topical losartan.
“We’ve got two years of experience with patients now, especially in Brazil, where the first patient in the world was treated and published. Now people are using it in India, Colombia and Europe too,” he says.
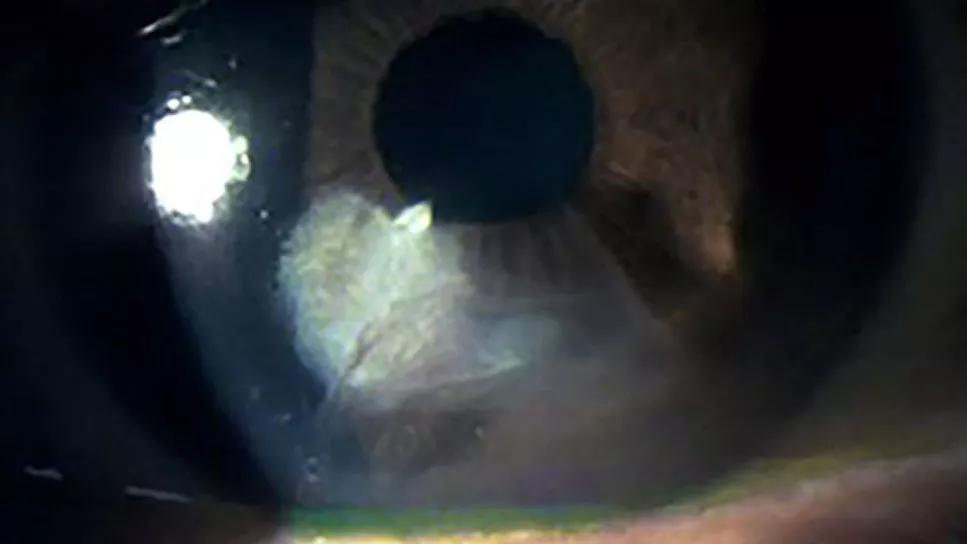
Feature image above: Corneal fibrosis following radial keratotomy performed many years earlier. Reprinted with permission from the Journal of Ocular Pharmacology and Therapeutics.
Advertisement
Advertisement

Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma

Study reveals more about the pathophysiology of Salzmann’s nodular degeneration

Identifies weak spots in the cornea before shape change occurs

Novel use of tPA reduces fibrin response in the eye

Researcher gives guidance for clinical trials

Untreated seropositive erosive RA led to peripheral ulcerative keratitis

Registry data highlight visual gains in patients with legal blindness

Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence