Our experts recap the most notable changes and developments
By Lars G. Svensson, MD, PhD; A. Marc Gillinov, MD; and Samir Kapadia, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
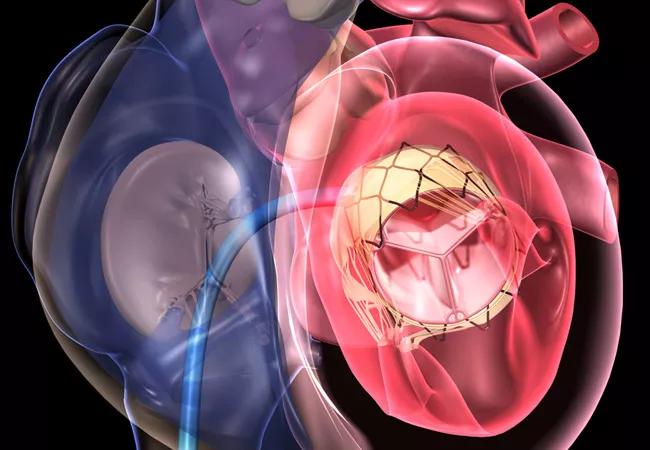
The American College of Cardiology (ACC) and American Heart Association (AHA) recently updated their joint guideline for the management of patients with valvular heart disease. Published in December in Circulation and the Journal of the American College of Cardiology, the 2020 guideline has added some new advice for earlier timing of procedures, but the document is mostly conservative. That’s reasonable, given the lack of long-term data for transcatheter aortic valve replacement (TAVR, or “TAVI” in the document) and mitral valve clips, for example.
For the first time, the guideline shows the average risk of death for seven Society of Thoracic Surgeons operation categories; these risks are some two to three times higher than those at Cleveland Clinic. The guideline also introduces criteria — based on outcomes, volume relationships and support — for Primary Valve Centers and for more advanced Comprehensive Valve Centers, with the recommendation that more advanced procedures be done at the latter centers. Additionally, new staging classifications have been introduced for specific valve diseases, based on symptoms and hemodynamics.
Below we summarize and reflect on a few of the most notable recommendations and changes in the new guideline, with a focus on the portions devoted to aortic valve disease. A subsequent post will focus on the guideline’s discussion of mitral valve disease.
The guideline classifies aortic valve stenosis (AS) into several stages:
Advertisement
Exercise testing in asymptomatic patients is deemed reasonable; if it demonstrates decreased exercise tolerance or induces a systolic pressure drop ≥ 10mmHg, aortic valve replacement (AVR) is reasonable.
In symptomatic patients, low-flow, low-gradient AS with reduced EF — or with normal EF if AS is the likely cause of symptoms — has been added as an indication for AVR.
For asymptomatic patients, added “reasonable” indications for AVR are Vmax ≥ 5m/s or gradient ≥ 60 mmHg, a B-type natriuretic peptide level > 3 times normal (> 300 pg/mL) or a progressive increase in velocity ≥ 0.3 m/s per year. Additionally, AVR may be considered for a progressive decline in EF to < 60%.
Note that the above indications are specifically for AVR in patients at low surgical risk and not for TAVR since the TAVR trials were in symptomatic patients with gradient ≥ 40 mmHg.
As in clinical practice, the recommendations are for joint decision making with the patient, with mechanical valve replacement for patients less than 50 years of age. For patients 50 to 65 years, choice should be individualized, although mechanical valves show a survival advantage. For patients over 65 years, AVR with a biological valve is reasonable.
In the recommendation for AVR versus TAVR, AVR is recommended for patients less than 65 years. For those aged 65 to 80 years, either AVR or TAVR (by transfemoral route) is recommended. Although the guideline recommends that patients older than 80 years or with life expectancy < 10 years should undergo TAVR (Class 1, Level A recommendation), this remains academically unproven since no prospective randomized trials nor post hoc analyses of the PARTNER trials or the Medtronic trials have addressed this specific question. Nevertheless, this is a matter for discussion with the patient. Notably, none of the pivotal clinical trials have addressed age cutoffs.
Advertisement
The guideline authors write that “compared with SAVR, TAVI results in higher rates of vascular complications, paravalvular regurgitation, permanent pacemaker implantation, and valve intervention, but most patients will consider that the advantages of TAVI outweigh these disadvantages.” Discussions with patients should note that in the PARTNER 3 trial in low-risk patients, stroke and death have equilibrated for TAVR versus AVR at one year, underscoring the need for longer-term follow-up. It should be noted that in intermediate-risk patients in PARTNER 2A, the risk of stroke and death with TAVR now exceeds that with AVR at five years (N Engl J Med. 2020;382:799-809). The authors also speculate that patients with low EF may benefit from TAVR because of “myocardial ischemia,” but there is no convincing evidence of this being a benefit from the randomized controlled trials.
The guideline notes that TAVR provided larger valve areas than AVR, although this held true only for the PARTNER 1 and 2 trials, when neither root enlargement nor selection of better-performing valves were allowed and when Edwards valves were the only ones approved. In PARTNER 3, with the allowance of root enlargement and selection of other valves, this finding was reversed, with AVR having larger areas, lower gradients and less patient-prosthesis mismatch.
The guideline recommends that renin-angiotensin blocker therapy (ACE inhibitor or angiotensin receptor blocker) be considered after TAVR (Class 2b, Level B-R recommendation). Previous AVR guidelines published by a team led by our group also recommended this following AVR in patients with a reduced EF.
Advertisement
Aortic valve regurgitation (AR) is also divided into stages in the new guideline:
Reasonable candidates for surgery for AR include asymptomatic patients with LVESD > 50 mm or indexed LVESD > 25 mm/m2 (Class 2a recommendation) and asymptomatic patients with progressive decline of EF or increasing LV dilation on serial echoes (Class 2b). TAVR should not be performed for AR (Class 3, Level B-NR recommendation). The indications for aortic valve repair are not discussed in detail but are essentially the same as for AVR in patients with AR.
Recommendations for management of bicuspid aortic valve remain unchanged from the 2016 guideline update, with surgery at a Comprehensive Valve Center recommended for patients with aortic diameter > 5.0 cm to 5.5 cm. We would recommend also using a ratio of >10 of cross-sectional area to height for particularly short or tall patients.
TAVR for severe symptomatic AS in patients with bicuspid valve is a Class 2b recommendation, i.e., can be considered after evaluating “patient-specific procedural risks, values, trade-offs, and preferences, when the surgery is performed at a Comprehensive Valve Center.” The guideline authors emphasize that bicuspid valve patients were excluded from the early TAVR trials and that, apart from paravalvular leaks, studies have raised concern about higher TAVR stroke risk in this population.
Advertisement
The guideline addresses the timing of intervention for patients with mixed AS and AR disease. AVR is recommended for symptomatic patients with Vmax ≥ 4 m/s or gradient ≥ 40 mmHg and for asymptomatic patients with Vmax ≥ 4 m/s and EF < 50%.
Lars G. Svensson, MD, PhD: “We congratulate the authors of the updated guideline for adding parameters that help cardiologists and surgeons better manage patients. Long-term data from prospective randomized trials will help define outcomes and better inform patients and physicians in their decision-making on the best approaches to treatment.”
Marc Gillinov, MD: “With more options to treat heart valve disease than ever before, it is incumbent upon physicians and their patients to take the time to discuss available treatments. It is particularly important that patients with additional issues beyond their valve disease — atrial fibrillation, coronary artery disease, ascending aortic aneurysm, mitral regurgitation — receive treatment for all of their conditions.”
Samir Kapadia, MD: “This updated guideline summarizes current understanding of valvular heart disease evaluation and management, but it is clear that the field is evolving rapidly with robust data from many randomized clinical trials — a relatively recent accomplishment in this field. In the current era, evaluation by a heart team made up of experienced and well-informed members is more important than ever in selecting appropriate treatment options for specific valvular heart diseases.”
Dr. Svensson is Chair of Cleveland Clinic’s Sydell and Arnold Miller Family Heart, Vascular & Thoracic Institute. Dr. Gillinov is Chair of the Department of Thoracic and Cardiovascular Surgery. Dr. Kapadia is Chair of the Department of Cardiovascular Medicine.
Advertisement

Scenarios where experience-based management nuance can matter most

Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients