Both patients experience improved visual acuity
By Peter K. Kaiser, MD, and Rishi P. Singh, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Retina specialists at the Cole Eye Institute recently reported in Ophthalmic Surgery, Lasers and Imaging Retina on two patients with traumatic macular holes with severe macular pathology that were treated with an inverted internal limited membrane (ILM) flap technique. Both patients experienced some degree of visual improvement.
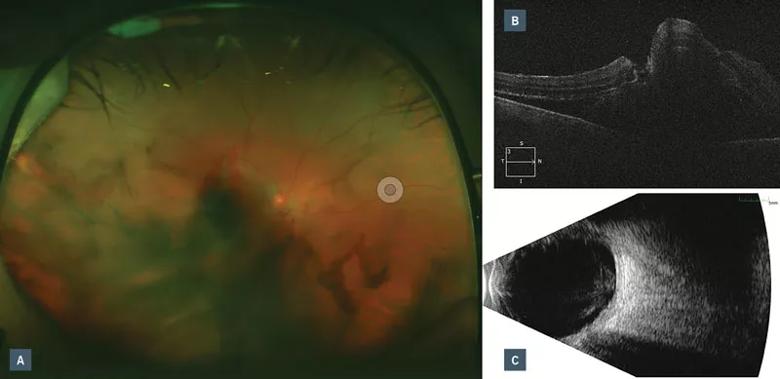
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ae698cdf-607e-424d-afc4-8ab11209ccc4/18-EYE-4343-R-Singh-Kaiser-CQD-Inset-1_jpg)
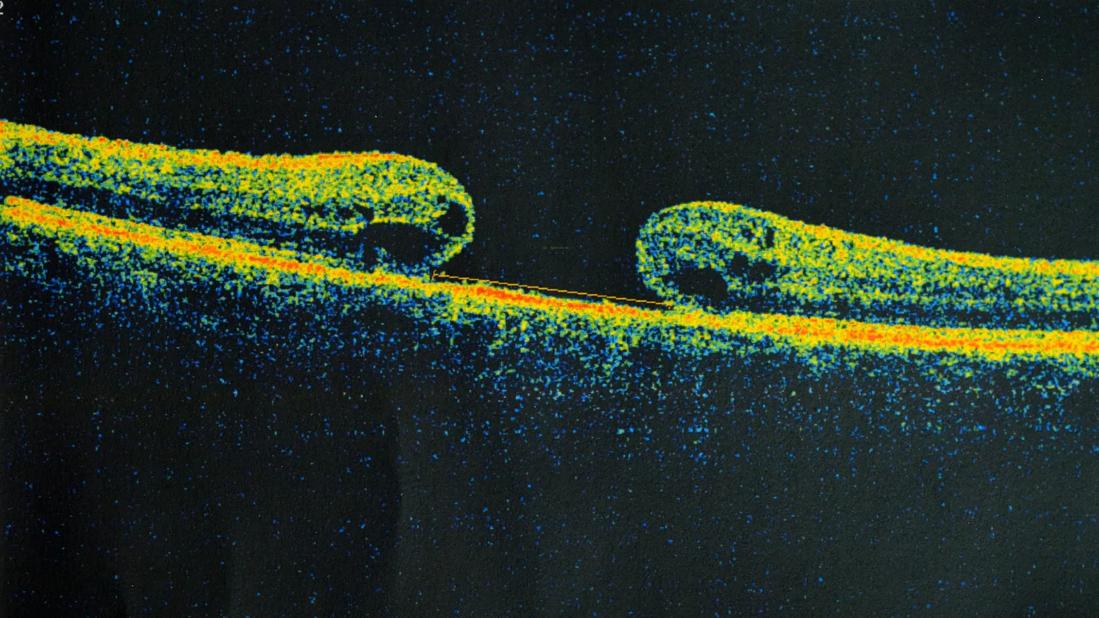
Figure 1. (a) Fundus photo with vitreous, subretinal, and subretinal pigmented epithelial hemorrhage. (b) Optical coherence tomography demonstrates macular detachment with a possible full-thickness macular hole. (c) B-scan ultrasonography displaying mobile vitreous opacities with elevated clumped opacities in the macular but without rhegmatogenous retinal detachment.
The first patient was a 39-year-old female who had been struck in the right eye by a baseball at a professional game three days earlier. Her vision in the eye was counting fingers only. As reported in the journal, she had a vitreous hemorrhage with subretinal and retinal pigment epithelial (RPE) hemorrhage and a choroidal rupture through the macula. On optical coherence tomography, she had a macular detachment with a possible full-thickness macular hole (FTMH). It was decided to follow the patient closely to allow the hemorrhages to resolve. Four months later, the vitreous hemorrhage had resolved, revealing two FTMHs ‒ one involving the fovea and the second temporal to it, overlying a choroidal rupture site.
Dr. Kaiser performed a pars plana vitrectomy (PPV) procedure with indocyanine green staining of the ILM, peeling of the ILM around both holes with preservation of a large temporal ILM flap that would cover both FTMH, air-fluid exchange and insuflation with C3F8 gas. The ILM flap was constructed on the temporal edge of the temporal eccentric macular hole so that during air-fluid exchange, the ocular fluidics would position the flap over both holes. Three months after surgery, both macular holes were closed and the patient had regained 20/150 vision.
Advertisement
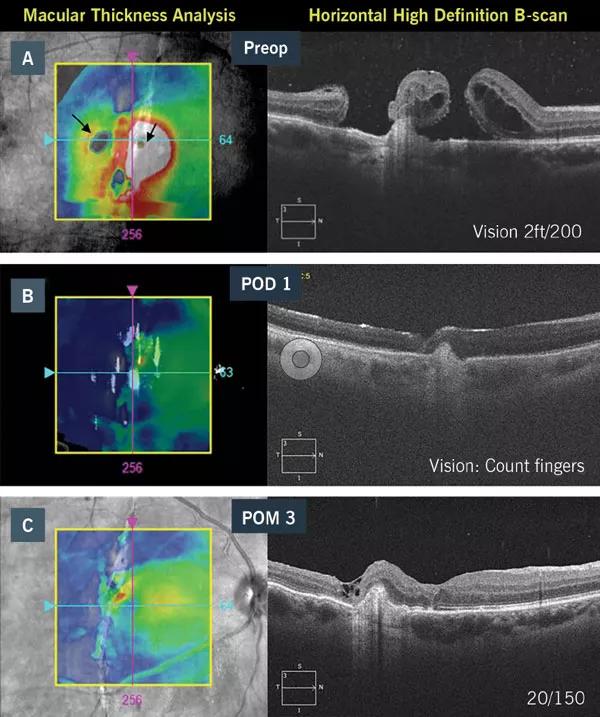
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b7c8e77b-47c4-4e9d-801e-2ab5101f258c/18-EYE-4343-R-Singh-Kaiser-CQD-Inset-2_jpg)
Figure 2. (a) Preoperative optical coherence tomography (OCT) demonstrates two macular holes overlying a choroidal rupture. (b) OCT under C3F8 on postop day 1. (c) Optical coherence tomography 3 months after surgery.
In the second case, a 22-year-old male presented one year after a motor vehicle accident in which an airbag struck his left eye. He reported a gradual decline in visual acuity since the accident. His vision in the affected eye was 20/250, with normal IOP.
Fundus exam revealed a pigmented macular scar with traumatic macular hole and vascular sheathing. OCT demonstrated dense vitreous condensation overlying a FTMH and a pigmented epithelial detachment. Over a three month period, his vision continued to decline to 20/500.
We performed a PPV with a large temporal ILM flap with placement assisted by intraoperative OCT, and C3F8 gas tamponade. Four months after the surgery, the traumatic macular hole was closed and the patient’s visual acuity had improved to 20/125.
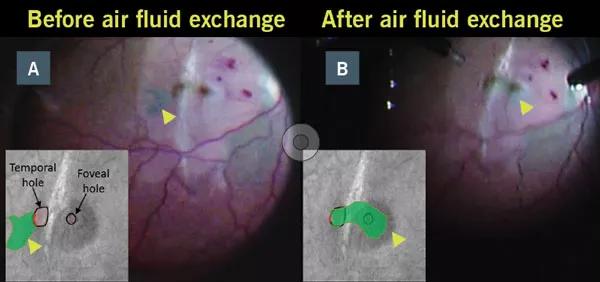
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/06c5900e-e270-4d85-98c7-1b4eee5f8342/18-EYE-4343-R-Singh-Kaiser-CQD-Inset-3_jpg)
Figure 3. (a, b) Fundus photo and schematic drawing of the internal limiting membrane flap before and after correct placement.
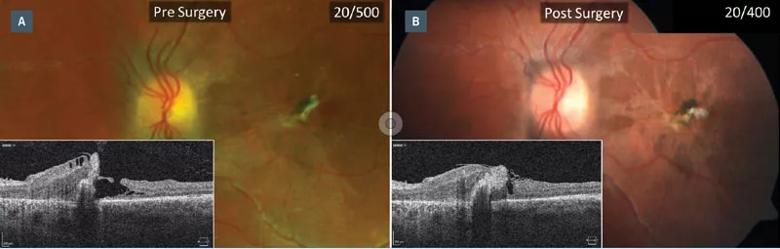
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6835861e-4f83-40a9-adc0-f6117fbd8bf5/18-EYE-4343-R-Singh-Kaiser-CQD-Inset-4_jpg)
Figure 4. (a) Fundus photo and optical coherence tomography (OCT) displaying full-thickness macular hole and pigmented epithelial
We have many tools available today to repair macular holes, including removal of the posterior hyaloid, epiretinal membrane, internal limiting membrane (ILM), and the addition of gas or silicone oil tamponade. However, there have been no controlled trials that compare the different options for trauma patients.
Advertisement
This report demonstrates two cases of FTMH with severe retinal pathology. In both cases, the ILM flap technique was employed and macular hole closure with improved visual acuity was achieved.
These results point to this approach as an effective treatment option. Of course, our report is retrospective and lacks a control group that underwent PPV with ILM removal without a flap applied to the hole. Future randomized trials would be needed to better evaluate whether PPV with and without ILM flap technique is an improved approach to the treatment of patients with traumatic macular holes.
Advertisement
Advertisement

Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma

Registry data highlight visual gains in patients with legal blindness

Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence

A look at emerging technology shaping retina surgery

A primer on MIGS methods and devices

7 keys to success for comprehensive ophthalmologists

Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs

Treatment options range from tetracycline injections to fat repositioning and cheek lift