Treatment options range from tetracycline injections to fat repositioning and cheek lift
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
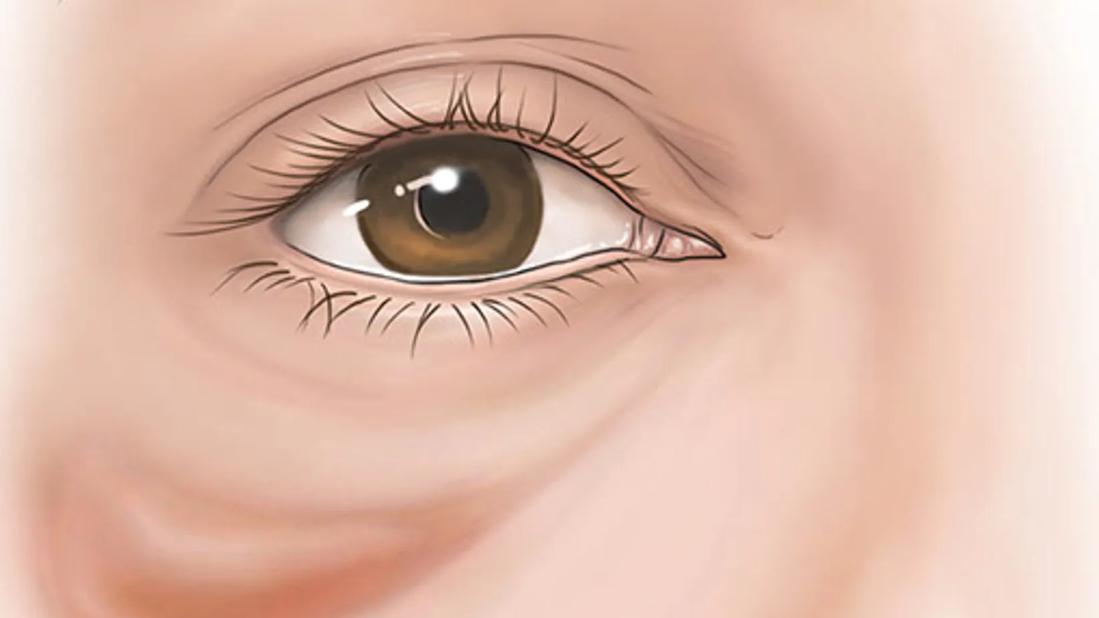
Festoons, or malar mounds, are pouches that appear on the cheekbones, under the lower eyelids. They are challenging to manage because:
The etiology of festoons involves laxity of tissue, including skin and the orbicularis oculi, as well as the weakening of the orbitomalar ligament, zygomatic cutaneous ligament and dermal attachments. This laxity combined with an unknown physiological phenomenon produces lymphatic stasis and the hallmark fluid retention of festoons.
While there is no cure for festoons, there is a range of treatment options that can improve their appearance. The following treatments have produced successful results in many of my patients.
One surgical option involves camouflaging the festoon with fat repositioning.
Through a transconjunctival incision, I perform blunt dissection to expose the arcus marginalis. Then I use a monopolar cautery instrument to make an incision through the periosteum, 1-2 mm inferior to the arcus marginalis. I also use the cautery instrument to perform the subperiosteal dissection. It works very well and is a quick way to raise the periosteum.
The most important factor when repositioning fat to camouflage festoons is the depth of the pockets. The pockets must be extremely deep so you can recruit fat into the area surrounding the festoon. This fat helps “rise the tide,” filling in hollows around the festoon.
Advertisement
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_3e5d3r5i/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Wide subperiosteal pocket during fat repositioning to camouflage a festoon.
I form sections of orbital fat into T-shaped pedicles: medially, centrally and sometimes laterally. The T shape allows each pedicle to spread into superior and inferior areas, creating great augmentation. These pedicles should be able to retain their T shape and maintain their position without any tension, meshing together to form a smooth area all around the festoon, thereby camouflaging it.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/055d92d4-6095-4b11-8fd6-38233fdb93c5/orbital-fat-festoon-surgery)
T-shaped pedicle of orbital fat.
I don't use suture fixation. I use the backside of 0.5 mm forceps to push the long pedicles of fat into the deep pockets. They are pinched in place under the edge of the periosteum, which creates stable fixation without sutures.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_p2fv90fx/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Surgical procedure to camouflage a festoon with fat repositioning.
A second surgical option involves resuspending and effacing the festoon with a cheek lift and skin removal. Cheek lift can suspend the festoon higher and redistribute it across a broader area, thereby making it appear less noticeable. The idea is to lyse the zygomatic cutaneous ligament and remove some skin to elevate and diminish the compartment in which the festoon can exist.
Subperiosteal cheek lifting begins with canthotomy and cantholysis, and then dissection continues under the tarsus. Dissection can be extended all the way to the caruncle for cases also involving fat repositioning.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a657f668-5d91-4875-a72a-0e68ef095098/conjunctival-incision)
Conjunctival incision just beneath the tarsus.
Similar to fat repositioning, I bluntly dissect towards the arcus marginalis. I use a monopolar cautery instrument to make an incision medially through the periosteum, 1-2 mm outside the arcus marginalis, and then use it to perform the subperiosteal dissection. The instrument will cauterize the zygomaticofacial and zygomaticotemporal foramina, which can leak slightly. This helps speed the dissection.
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/914ce5bf-fbd6-4d5f-9363-58cf9af39784/subperiosteal-dissection)
Using the monopolar cautery instrument to perform subperiosteal dissection.
To lyse the zygomatic cutaneous ligament, it is important to dissect well underneath the festoon — all the way medially to the nerve, laterally to the zygoma, and inferiorly up to 4 cm beneath the rim. Once the dissection proceeds far enough inferiorly, I make an incision through the periosteum to completely free the cheek to allow for excellent mobilization of the festoon. The entire dissection can be performed in minutes.
Grasping the SOOF (suborbicularis oculi fat) and elevating it lifts the festoon. Then I remove the extra skin (with a skin pinch or skin flap) to reduce the festoon’s compartment. Elevating and effacing the festoon and shortening the eyelid often can provide overall cosmetic improvement.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/99840f0f-a1a1-4123-9d98-47737a748cdf/skin-pinch-festoon-surgery)
Skin pinch to remove extra skin and reduce the festoon’s compartment.
An alternative to surgery, sclerosing the festoon with tetracycline can be performed either in the operating room or in the office. Injecting tetracycline throughout the festoon damages the mesothelial surfaces, which stimulates fibroblast proliferation and leads to collagen and fibrin deposition in the inflamed pleural space. Basically, it creates scar tissue beneath the festoon to seal the fluid blister and prevent more fluid accumulation.
While it does offer a less-invasive treatment option, injecting tetracycline:
Advertisement
Combining tetracycline injection with surgical techniques can yield some of the best results, in my opinion.
In summary, festoon treatment can be humbling, but there is a range of treatment options — from in-office injections to surgical procedures or a combination of treatments — to match each patient’s level of commitment to improving their appearance.
Dr. Perry is an ophthalmic plastic and reconstructive surgeon at Cleveland Clinic Cole Eye Institute.
Advertisement
Advertisement

A roundtable discussion on aesthetic surgery

Personalized reconstruction is an alternative to leg amputation or flail limb

Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma

Registry data highlight visual gains in patients with legal blindness

Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence

A look at emerging technology shaping retina surgery

A primer on MIGS methods and devices

7 keys to success for comprehensive ophthalmologists