Findings reveal lower survival, fewer interventions relative to primary MR
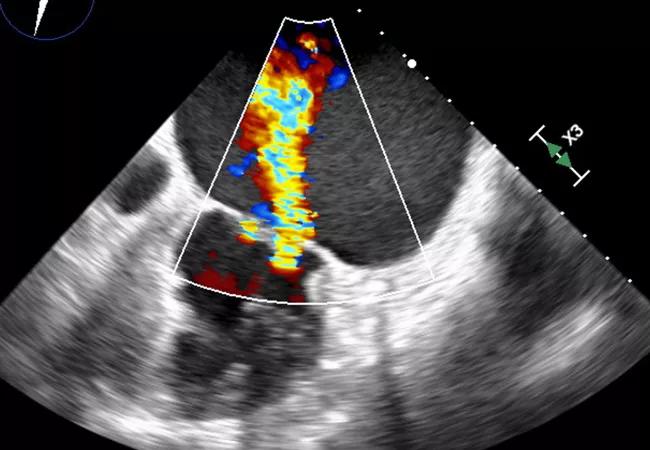
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ceb41563-66a0-40e6-aea6-2f04bee33dea/21-HVI-2108077-CQD-Atrial-Functional-Mitral-Regurgitation-Hero_jpg)
echocardiogram showing severe atrial functional mitral regurgitation
Atrial functional mitral regurgitation (AFMR) has been a neglected clinical entity. Although it has been described for at least a decade, AFMR is underrecognized, undertreated and rather poorly understood.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
That might be starting to change, however, with the recent publication of a Cleveland Clinic study in JACC: Cardiovascular Imaging (2021;14:797-808) believed to represent the largest cohort of patients with severe AFMR identified by transesophageal echocardiography (TEE) reported to date.
“AFMR is neither primary mitral regurgitation (MR), which is a valve problem, nor the typical functional or secondary MR, which is ventricular in origin. Rather, it is functional MR of atrial origin,” says the study’s corresponding author, Serge Harb, MD, staff cardiologist in Cleveland Clinic’s Section of Cardiovascular Imaging.
“Patients with AFMR have not been studied separately in clinical trials, and literature about AFMR is sparse,” Dr. Harb continues. “As a result, there are no guidelines to advise physicians on how to approach this problem, which carries a poor prognosis.”
“The mitral valve is equipped to withstand the highest pressure in the heart,” says study co-author Samir Kapadia, MD, Chair of Cardiovascular Medicine. “This study characterizes the mechanism and contribution of left atrial dilatation on mitral apparatus dysfunction in a large Cleveland Clinic population. This mechanistic insight is critical for proper and timely interventions to prevent and treat mitral regurgitation.”
The growing number of patients presenting with MR and normal ventricular function in the absence of leaflet pathology prompted the Cleveland Clinic team to better define the clinical entity they were seeing.
Advertisement
They screened all patients who had undergone TEE at Cleveland Clinic between 2011 and 2018 for severe MR with preserved left ventricular function. After patients with endocarditis, cardiomyopathy or prior mitral valve intervention were excluded, a cohort of 283 patients remained. Of this cohort, 39 (14%) had AFMR and 244 (86%) had primary MR.
When the AFMR and primary MR groups were compared, patients with AFMR had significantly higher rates of hypertension, diabetes mellitus, long-standing atrial fibrillation, pacemaker placement and prior nonmitral cardiac surgery.
“Atrial fibrillation and diastolic dysfunction were the main risk factors,” says Dr. Harb.
Over a median follow-up of 22 months, mortality was significantly higher among patients with AFMR compared to those with primary MR (41.0% vs. 18.9%; P = 0.004). On multivariable regression analysis, AFMR was independently associated with mortality (OR = 2.61; 95% CI, 1.17-5.83; P = 0.02).
Patients with AFMR also were twice as likely as their primary MR counterparts to be hospitalized for heart failure (51.3% vs. 25.4%; P = 0.002)
AFMR is distinguished by atrial dilation and annular remodeling. “Mitral annular dilation with insufficient leaflet remodeling is the most commonly described feature,” notes Dr. Harb. “Malcoaptation of the leaflets results in a central jet of regurgitation that can be clearly seen on transesophageal echo.”
In other cases, the posterior annulus is stretched outward and herniates over the left ventricular free wall. This causes tethering of the posterior leaflet and a predominantly posterior jet of regurgitation.
Advertisement
“Typically, AFMR requires transesophageal echo to ascertain,” Dr. Harb explains (see Figure). “However, the diagnosis of MR should start with a transthoracic echo and proceed to transesophageal echo if an unusual form of MR is suspected, in which case transesophageal echo can help elucidate the features of AFMR.”
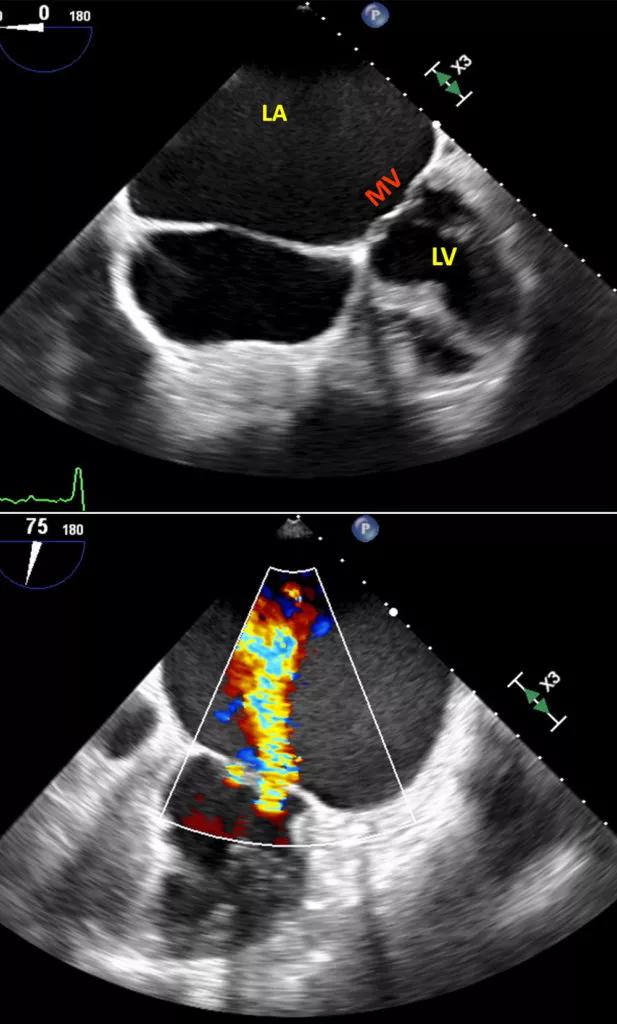
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c80f3150-a095-4d17-bf57-a6f8abd7ae96/21-HVI-2108077-CQD-Atrial-Functional-Mitral-Regurgitation-Inset-617x1024_jpg)
Figure. Top transesophageal echocardiogram (TEE) shows a markedly enlarged left atrial (LA) cavity with no mitral valve (MV) leaflet pathology and a normal left ventricle (LV). Bottom TEE shows severe atrial functional (or secondary) mitral regurgitation (AFMR).
Surgery can improve outcomes in AFMR. Compared with conservative management, mitral valve surgery was associated with improved survival in AFMR (log-rank P = 0.021). Also, none of the 10 AFMR patients who underwent surgical mitral valve repair developed significant MR on follow-up or needed further mitral interventions.
Nevertheless, patients with AFMR were less likely than their primary MR counterparts to undergo a mitral intervention of any kind (59.0% vs. 83.6%; P = 0.001). Dr. Harb attributes this to increased risk conferred by older age, significant comorbidities and frequent prior cardiac surgery — as well as a lack of guidelines for managing these patients.
“Distinguishing atrial functional MR from other causes of mitral regurgitation is very important,” observes study co-author Marc Gillinov, MD, Chair of Thoracic and Cardiovascular Surgery at Cleveland Clinic. “In many cases, an operation that includes both mitral valve repair and a maze procedure for atrial fibrillation reduces symptoms and improves patient quality of life.”
Advertisement
Dr. Harb notes that comprehensive guidance on the best way to manage patients with AFMR “is something for future research to answer.”
In the meantime, he says, preventing the onset of severe MR is the best option. “Practice aggressive rhythm control to restore sinus rhythm and treat diastolic dysfunction before severe MR develops,” he advises. “If you cannot prevent it, and the patient develops severe AFMR, mitral valve repair or replacement may improve survival.”
Advertisement
Advertisement
After four decades, refinements to the gold standard of bypass continue as new insights emerge
Why definitive surgical closure is the gold standard, and new ways to make it possible
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Cleveland Clinic’s new dedicated program offers nuanced care for a newly recognized cardiovascular risk factor
Scenarios where experience-based management nuance can matter most
Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics
How Cleveland Clinic is using and testing TMVR systems and approaches
NIH-funded comparative trial will complete enrollment soon