Fast visualization of subtle flow abnormalities makes surgery more precise

By Alex M. Witek, MD, and Mark D. Bain, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 63-year-old man presented to his primary care physician with headaches. MRI showed an incidental, unruptured aneurysm. He was referred for evaluation to Cleveland Clinic, where a diagnostic cerebral angiogram was obtained to better characterize the aneurysm. This demonstrated a 14-mm aneurysm at the right middle cerebral artery (MCA) bifurcation (Figure 1).
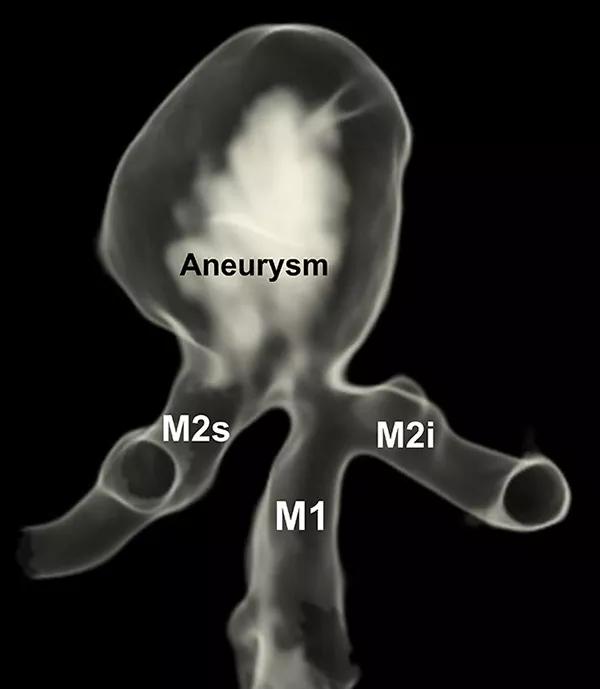
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/94f4dba6-7fc4-46d4-b61d-e2b0d25e2f10/17-NEU-673-Bain-inset1_jpg)
Figure 1. Three-dimensional angiogram of the right middle cerebral artery (MCA) bifurcation demonstrates a saccular aneurysm arising along the origin of the M2 superior trunk. (M1 = M1 segment of MCA; M2s = MCA superior trunk; M2i = MCA inferior trunk)
Treatment was recommended to reduce his risk of future aneurysm rupture. The aneurysm incorporated a branch vessel into its neck, so endovascular therapy would be challenging and might have carried a significant risk of stroke. For this reason, microsurgical clipping was recommended.
A standard frontotemporal craniotomy was performed, preserving the right superficial temporal artery (STA) for possible bypass. The Sylvian fissure was opened using microsurgical dissection, and the aneurysm came into view at the MCA bifurcation. Figure 2 shows the view through the surgical microscope, including the M1 parent vessel, the superior M2 trunk and the inferior M2 trunk. The aneurysm neck was located asymmetrically along the origin of the superior trunk.
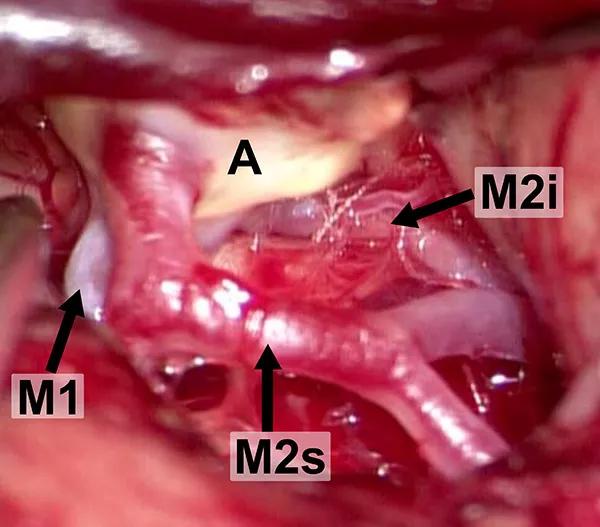
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/dfe7d0cc-bb7a-4430-be0d-e56b80f16317/17-NEU-673-Bain-inset2_jpg)
Figure 2. Intraoperative microscopic view of the MCA bifurcation seen through the Sylvian fissure. (M1 = M1 segment of MCA; M2s = MCA superior trunk; M2i = MCA inferior trunk; A = aneurysm)
Advertisement
A titanium clip was placed across the neck of the aneurysm. After clip placement, indocyanine green (ICG) video angiography was performed and appeared to show no residual aneurysm filling and patency of both branch vessels.
We then used the FLOW® 800 analysis tool (Carl Zeiss Meditec AG, Oberkochen, Germany) to analyze the flow, which revealed delayed filling of the superior MCA territory (Figure 3) despite the absence of obvious stenosis on video replay. A digital subtraction angiogram (DSA) confirmed slow filling of the superior division.
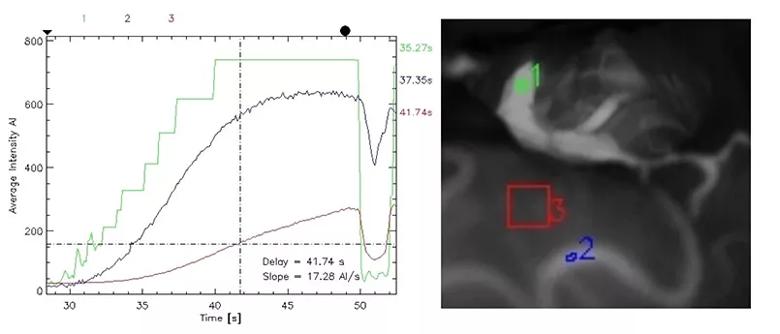
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6f213821-d606-4403-930d-649f8122b8e5/17-NEU-673-Bain-inset3_jpg)
Figure 3. FLOW 800 analysis after application of the clip to the aneurysm neck (before bypass) demonstrating slow filling of the superior division. The graph on the left displays the fluorescence intensity-time curves for three regions of interest, the locations of which are shown in the photo on the right (region 1 [green] = superior MCA trunk; region 2 [blue] = M4 frontal branch; region 3 [red] = inferior frontal gyrus).
After we attempted to reposition the clip, it became apparent that it would be difficult to simultaneously occlude the aneurysm while maintaining patency of the branch vessel. We therefore proceeded with a bypass via end-to-side anastomosis of the STA to the superior M2 trunk. The clip was then repositioned so that it excluded the aneurysm (along with superior trunk) from the circulation while the bypass provided flow replacement to the superior division. Repeat ICG injection and FLOW 800 analysis revealed brisk filling of the superior MCA territory (Figure 4).
Advertisement
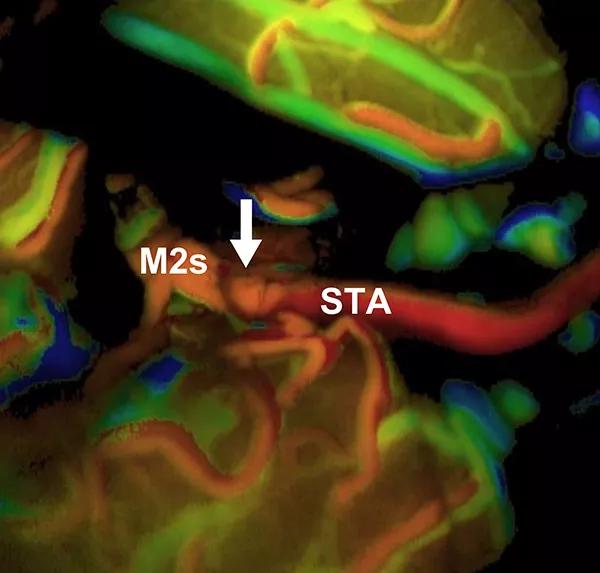
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e9a55e9f-7fc4-493c-84b7-f1acff905dc3/17-NEU-673-Bain-inset4_jpg)
Figure 4. FLOW 800 time-to-arrival map after the bypass and occlusion of the aneurysm (and MCA superior trunk) with a clip. The map demonstrates brisk filling of the superior division via the bypass. The superficial temporal artery (STA) bypass graft, recipient MCA superior trunk (M2s) and end-to-side anastomosis (arrow) are indicated.
The patient awoke from surgery at his neurologic baseline. He underwent routine postoperative care and was discharged home. He made an excellent recovery and continues to do well two months later.
Although the development of endovascular devices and techniques has allowed us to safely treat many types of aneurysms without a craniotomy, there are still many aneurysms (such as this one) that are treated more safely with open surgery.
Open aneurysm surgery has benefited from a number of technological improvements over the past few decades that have increased its efficacy and safety. ICG video angiography, a technique first described in 2003 (Raabe et al., Neurosurgery. 2003;52[1]:132-139), involves intravenous injection of a fluorophore (ICG) that is visualized as it passes through the intracranial circulation by exciting the surgical field with a near-infrared source and detecting its fluorescence with an infrared camera. FLOW 800 is a newer software package that provides time-resolved quantitative analysis of ICG angiography. The resulting data can be displayed in multiple ways, including time-to-arrival maps (as in Figure 4) and time-intensity curves for selected regions of interest (as in Figure 3).
Advertisement
This case demonstrates the utility of FLOW 800 technology for aneurysm surgery. Visual inspection of the aneurysm and its associated vessels is not a reliable way to determine optimal clip placement because it does not show the arterial lumen. A clip that appears well-placed from an extraluminal perspective can actually be causing significant stenosis of the parent vessel, especially if the aneurysm neck is thick or calcified.
Until now, the best available methods for seeing inside the vessel lumen during surgery have included DSA and qualitative ICG angiography. Although DSA is considered the gold standard for vessel imaging, it takes time to set up and perform, which can be enough to cause a stroke if there is significant vessel stenosis. Routine ICG video angiography allows us to see inside the blood vessels in a much quicker fashion, making it a valuable supplement and/or alternative to DSA.
ICG was previously a purely quantitative procedure, but the recent addition of FLOW 800 provides valuable quantitative data. This technology can reveal subtle flow abnormalities not evident on video replay, and the post-processing required to obtain these data takes less than a minute.
We have found FLOW 800 to be useful for aneurysm and bypass surgery, and we expect it will also provide valuable information during surgery for arteriovenous malformations. The utility of FLOW 800 in this case demonstrates how new technologies have made surgery safer and more precise for our patients.
Dr. Witek is a resident in Cleveland Clinic’s Department of Neurosurgery.
Advertisement
Dr. Bain is a staff surgeon in the Department of Neurosurgery and Cleveland Clinic’s Cerebrovascular Center.
Advertisement

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Tool helps patients understand when to ask for help