Patients with iliac extension may need hybrid or endovascular interventions
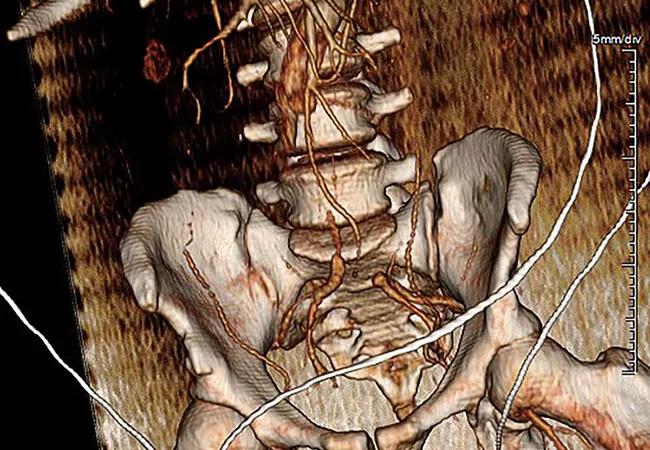
Most cases of type A aortic dissection (TAAD) with acute lower extremity ischemia (ALI) resolve with proximal aortic repair. But extension of dissection into zone 11 (i.e., iliac involvement) increases the risk of amputation and mortality, and may need to be addressed with hybrid and endovascular interventions using a multidisciplinary team approach. So recommend Cleveland Clinic specialists in a study published in the Journal of Vascular Surgery describing management practices and outcomes of this rare presentation based on a series of 81 patients they treated over nearly a decade.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Ascending aortic dissection with distal malperfusion is a complex, high-risk presentation,” says study co-author Eric E. Roselli, MD, Surgical Director of Cleveland Clinic’s Aorta Center. “Multidisciplinary management with emergency primary aortic repair and additional peripheral revascularization can improve outcomes, especially when delivered in a timely manner that includes preoperative and perioperative strategic discussion among team members.”
TAAD (defined as acute aortic dissection involving the ascending aorta) is a catastrophic event requiring emergency surgery. It is associated with perioperative mortality rates as high as 30% or 40% when clinical ischemia is part of the presentation. Concomitant ALI reportedly occurs in about 7% to 15% of cases and increases the risk of mortality and limb amputation.
Although a few small case series have been published, standardized management strategies for such patients have not been established. To shed light on the many unanswered questions in this setting, the current study was designed to evaluate the incidence, clinical presentation, dissection morphology, treatment strategies and outcomes of patients undergoing proximal aortic repair for TAAD with ALI. The risk factors and impact of additional revascularization procedures were also examined.
Out of 463 patients identified who underwent proximal aortic repair for DeBakey extent 1 TAAD at Cleveland Clinic from January 2010 through December 2018, 81 patients (17%) presented with ALI.
Advertisement
Notable aspects of these 81 patients’ presentation included the following:
Key aspects of these patients’ management included the following:
In-hospital mortality among these patients with TAAD and ALI was 21% (17/81), and three patients (4%) had major amputation.
Analysis of risk factors revealed the following:
While recent reviews in the literature have reported in-hospital mortality rates of approximately 15% to 20% for patients presenting with TAAD, these rates have consistently been between 5% and 10% in the Cleveland Clinic experience. Similarly, other reports have typically described higher mortality rates for patients presenting with ischemia than what was seen in the current study, which demonstrated a mortality rate of 21% for patients presenting with combined TAAD and ALI.
Advertisement
The study authors offer guidance on best practices for improving outcomes of patients with this complex presentation of TAAD plus ALI, specifically addressing the following issues.
Timing of proximal aortic repair vs. peripheral reperfusion. Whether to first perform proximal aortic repair or resolve the malperfusion remains controversial. Risk of death from aortic rupture must be weighed against the risk of malperfusion-related organ failure. In this study, three of 24 patients underwent revascularization before proximal aortic repair, and two of them died in the hospital. “This is an especially difficult situation, as patients with TAAD and ALI face multiple threats to survival,” says Francis Caputo, MD, Vascular Surgery Director of Cleveland Clinic’s Aorta Center. “We use a complication-directed strategy with the goal of addressing the most threatening issue first. The highest-risk patients are those who experience delays in diagnosis or get referred for transfer late in the course of the ischemic process.”
Evolving repair strategies. During the study period (2010-2018), the primary approaches to proximal aortic repair were limited ascending and hemiarch replacement. However, during the more recent half of the study period, frozen elephant trunk repairs were used with increasing frequency. “Currently, we prefer an extended repair using a simplified frozen elephant trunk strategy for TAAD patients presenting with distal malperfusion,” says Dr. Roselli. “The study showed that this strategy facilitated additional endovascular interventions in select cases without worsening outcomes. We also have augmented our cardiopulmonary bypass strategies with limb perfusion circuits to provide early limb reperfusion and reduce ischemic time during the course of conducting the proximal aortic repairs.”
Advertisement
Revascularization strategies to optimize true lumen perfusion.Thoracic aortic stent placement was the most common additional revascularization procedure for persistent true lumen collapse after proximal repair; it is often sufficient to resolve limb ischemia and renovisceral malperfusion by addressing the dynamic component of malperfusion. Open, endovascular or hybrid techniques were all effective at achieving successful outcomes. “Whichever strategy is ultimately chosen, we postoperatively verify complete reperfusion,” says Dr. Caputo. “This involves confirming distal true lumen expansion and reestablishment of visceral and limb perfusion using angiography and intravascular ultrasonography.”
Mesenteric malperfusion as a marker of severe risk. The study found that the need for additional revascularization predicted lower amputation-free survival. Also of note, there was a higher prevalence of mesenteric malperfusion in patients who required additional revascularization. “Renovisceral malperfusion is among the most detrimental forms of ischemia and a strong risk factor for early mortality,” observes study co-author Venu Menon, MD, Section Head of Clinical Cardiology and Director of the Cardiac Intensive Care Unit. “While proximal aortic repair of TAAD results in resolution of acute lower extremity ischemia in most cases, it is important to recognize this complication.”
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more