Definitions give new weight to secondary and composite endpoints, quality-of-life metrics
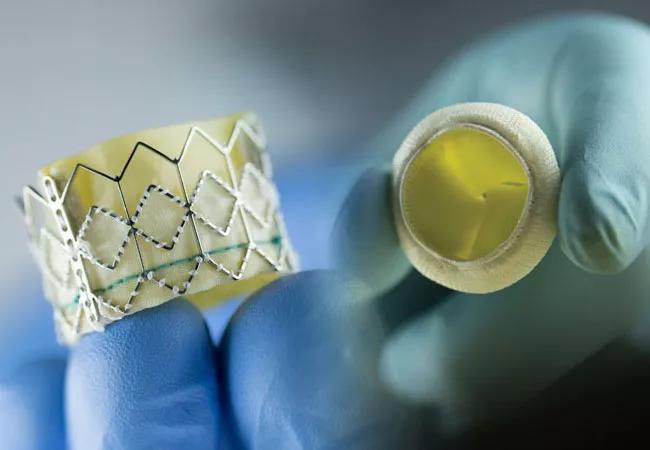
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/bf19104f-de78-42c1-84c7-82d350060e5c/21-HVI-2168809-CQD-VARC-3-endpoint-definitions_jpg)
photo of aortic valve prostheses
Contemporary aortic valve research is a fast-evolving field. Clinical investigations increasingly involve patients who are younger and have a greater variety of clinical indications and levels of disease severity. And comparisons of all kinds are being made, whether between transcatheter and surgical aortic valve replacement (TAVR/SAVR) or among various devices or other technologies used for either TAVR or SAVR.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In response, the Valve Academic Research Consortium (VARC) recently updated its standardized definitions of clinical endpoints for aortic valve clinical research. The new definitions, which build on the group’s first set of definitions issued in 2011 (known as VARC) and an update in 2012 (VARC-2), were co-published in the Journal of the American College of Cardiology and the European Heart Journal.
The update — referred to as VARC-3 — reflects recent clinical trials’ heavier focus on secondary endpoints, composite safety and efficacy endpoints, and quality-of-life assessments. VARC-3 also embraces the need to define new endpoints and reevaluate definitions of existing endpoints used by the aortic valve research community around the globe.
“The use of clinically relevant endpoints with consistent definitions, appropriate to the size and type of the clinical study, are essential to collecting, adjudicating and reporting large randomized trials and rigorous observational studies,” says Samir Kapadia, MD, Chair of Cardiovascular Medicine at Cleveland Clinic and a member of the VARC-3 writing committee.
As a leading trial site for aortic valve research, Cleveland Clinic has a clear interest in ensuring updated definitions to support accurate interpretation of outcomes. “We participated in VARC-3 so we could provide our opinion on definitions that make sense clinically,” says Dr. Kapadia, who was joined on the writing committee by Eugene Blackstone, MD, Head of Clinical Investigations in Cleveland Clinic’s Miller Family Heart, Vascular & Thoracic Institute.
Advertisement
“Given the large investments of time and resources that go into a clinical trial, it’s important to make sure the trial isn’t compromised by criticisms stemming from use of questionable endpoint definitions,” Dr. Kapadia adds.
Based on clinical knowledge gained since VARC-2 was issued, VARC-3 added definitions for the following:
“Lack of standard definitions for these endpoints has made comparisons difficult,” Dr. Kapadia explains. “For example, in January 2019 we published a systematic review on the durability of all 17 available bioprosthetic valves for SAVR, and we found that 11 different definitions of structural valve deterioration had been used.”
Moreover, modifications were made to definitions of the following:
“These definitions now have specific criteria and are very detailed,” Dr. Kapadia notes.
He suggests that clinicians begin absorbing the vast amount of information included in the VARC-3 document by looking at the tables and seeing what definitions are used. “If you don’t understand the definitions, look at the references to learn why we defined a term the way we did,” he advises.
Advertisement
The VARC-3 update built on months of work by more than 75 individuals from academic medical centers, professional societies, the FDA and industry focused on evaluating the use of VARC definitions in clinical research to ensure clinical relevance. The writing committee — comprising 23 cardiologists and cardiac surgeons from the larger group, all representing academic centers or professional societies from the U.S., Canada and Europe — then independently drafted the updated VARC-3 definitions. The entire process took more than three years.
Although VARC-3 has generated some controversy, Dr. Kapadia says all definitions were vetted and approved by all authors, the major cardiovascular societies, the FDA and industry representatives.
“We did not want to be biased, so we had very open discussions on what individuals considered limitations of these definitions,” he observes. “Of course, some people had to compromise in some areas, but everyone wanted to do right by this project.”
Dr. Kapadia expects VARC-3 to have a substantial impact on future clinical trials in aortic valve disease. “From now on, all trials must use these definitions,” he says. “If a trial does not, its results will not carry adequate authority to shape practice.”
Now that aortic valve research terminology has been updated, Dr. Kapadia and his international colleagues have turned their attention to updating endpoint definitions for clinical research involving the mitral valve (MVARC) and establishing such definitions for research involving the tricuspid valve (TVARC).
Advertisement
Advertisement
A new CME opportunity in Chicago, May 15-16
After four decades, refinements to the gold standard of bypass continue as new insights emerge
Why definitive surgical closure is the gold standard, and new ways to make it possible
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Cleveland Clinic’s new dedicated program offers nuanced care for a newly recognized cardiovascular risk factor
Scenarios where experience-based management nuance can matter most
Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics
How Cleveland Clinic is using and testing TMVR systems and approaches