High-magnitude curves pose challenges, but experience can yield success
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
C.R. presented to Cleveland Clinic at age 27 complaining of predominantly axial back pain. She had a known congenital kyphosis of the thoracolumbar junction that had been followed for many years at another hospital. Over approximately two years she developed debilitating back pain and some activity-related bilateral lower-extremity pain.
Examination, including anteroposterior and lateral X-rays (Figure 1), confirmed a severe congenital kyphosis (130 degrees) at the thoracolumbar junction, lumbar hyperlordosis and thoracic hyperlordosis.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e4c5dadd-ff18-41e6-a405-123ba8fbd3ed/17-NEU-672-Orr-inset1_jpg)
Figure 1. The patient’s preoperative standing X-rays. The anteroposterior view (left) shows some coronal plane deformity. The lateral view (right) shows a 130-degree congenital kyphosis.
High-magnitude curves such as this present many challenges for surgical treatment. The bony anatomy is altered due to the underlying congenital anomalies as well as the adaptive changes that have occurred over years in such an abnormal posture. In addition, the spinal cord is tightly opposed to the vertebral bodies at the apex.
The surgical plan was an all-posterior approach with resection of the abnormal vertebra at the apex of the kyphosis and a long segmental instrumentation. This procedure is called a vertebral body resection and essentially results in separation of the spinal column into two mobile segments with only the dura and spinal cord staying intact across the ensuing defect.
Difficulties were anticipated in removing the vertebral body with the cord in such proximity. In cases like this it is also difficult to determine the optimal length of the spinal column after resection. If the spine is shortened too much, there can be kinking of the spinal cord, leading to a spinal cord injury. If the column is lengthened too much, stretching of the cord can result and likewise lead to neurologic injury. Placement of hardware is also difficult, given the abnormal trajectories for pedicle screws involved.
Advertisement
The use of intraoperative spinal cord monitoring with somatosensory and motor evoked potentials greatly assists the surgeon in safely resecting the vertebral body and restoring spinal alignment without compromising spinal cord function. In a case such as this, the ability to obtain an intraoperative CT scan and merge it with an image-guided navigation system makes it much easier to place instrumentation while also helping guide the surgeon in complete resection of the vertebral bodies across the apex. The anterior column is then reconstructed with an expandable interbody cage and long-segment posterior instrumentation.
Figure 2 shows an intraoperative lateral X-ray from this patient’s case with a combination of temporary and definitive hardware in position. The surgery took about 8.5 hours. Unfortunately, the postoperative course was complicated by a wound infection, which was treated with operative irrigation debridement and a six-week course of intravenous antibiotics.
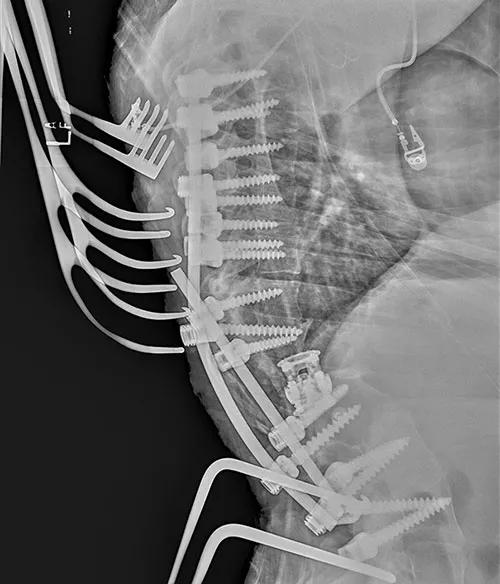
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e1cc0bfd-d0d1-4634-a4ad-4bbcb40113ea/17-NEU-672-Orr-inset2_jpg)
Figure 2. Intraoperative lateral X-ray showing a combination of temporary and definitive hardware after initial correction of the deformity.
At her most recent follow-up, six months after surgery, the patient was almost completely pain-free, had returned to full unrestricted activities and reported being very happy with her clinical status. Figure 3 shows her X-rays taken at that time.
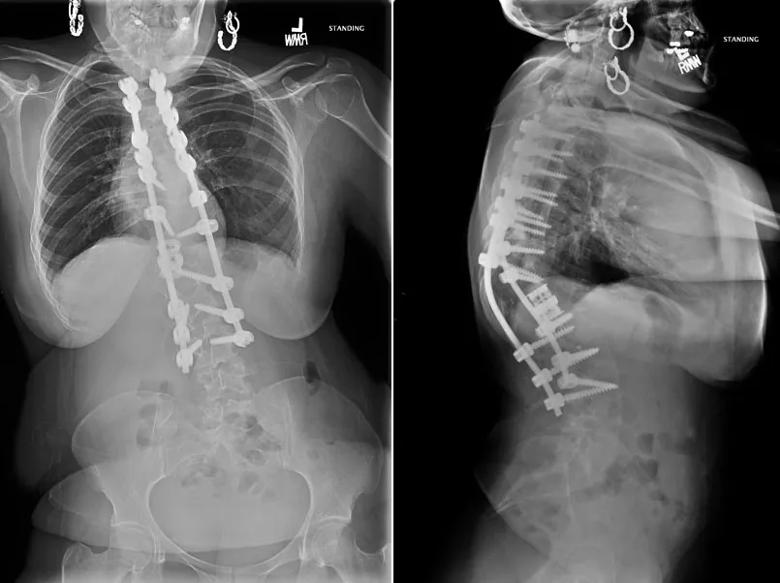
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e146b37c-29f1-47cd-9bdb-b99ffde6ab89/17-NEU-672-Orr-inset3_jpg)
Figure 3. X-rays taken six months postoperatively. The anteroposterior image on the left shows some persistent coronal plane malalignment while the lateral image on the right shows the final hardware construct and good sagittal alignment.
Advertisement
Surgeries for high-magnitude spinal deformities are among the most complex and challenging that can be performed. They are best done at centers with a large experience in these types of operations and access to a wide variety of advanced surgical techniques. Although these procedures carry relatively high risks, when successful they can result in major improvements in a patient’s quality of life.
Dr. Orr (orrd@ccf.org) is a spine surgeon in Cleveland Clinic’s Center for Spine Health.
Advertisement
Advertisement

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Tool helps patients understand when to ask for help