New study details trends in alternative-access TAVR from Cleveland Clinic
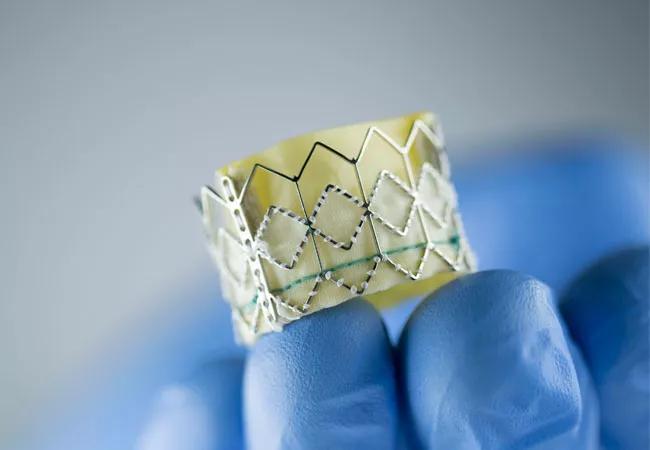
For patients who need transcatheter aortic valve replacement (TAVR) but whose anatomy precludes inserting the catheter through the femoral artery, the transaxillary approach has become the preferred alternative at Cleveland Clinic. The health system’s outcomes with transaxillary TAVR are comparable to those with transfemoral TAVR and superior to those with approaches that involve cutting into the chest, i.e., transapical and transaortic access. So finds a recent study published in Annals of Thoracic Surgery (2021;112:1877-1885) describing the evolution and outcomes of alternative-access TAVR at Cleveland Clinic.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“In the modern era, about 5% to 10% of TAVR patients require access with a method other than the standard transfemoral route,” says the study’s corresponding author, James Yun, MD, PhD, of Cleveland Clinic’s Department of Thoracic and Cardiovascular Surgery.
Typically the need for an alternative access route stems from narrowness, tortuosity or excessive calcification of the femoral or iliac arteries or the aorta. For patients with such anatomy, the alternatives include going through the apex of the left ventricle or through the aorta (both of which necessitate opening the chest cavity) or, increasingly, cutting down in the armpit to expose the axillary artery (i.e., the transaxillary approach).
While transapical access was the leading alternative to the transfemoral approach in the PARTNER clinical trials that helped establish TAVR, this approach was found to be associated with elevated rates of morbidity and mortality. This spurred interest in additional approaches, including transcarotid and transcaval routes in addition to the aforementioned transaortic and transaxillary approaches. The Cleveland Clinic researchers retrospectively reviewed their TAVR cases since introduction of the procedure to assess temporal trends and compare outcomes and complications among approaches.
During the 13-year study period (January 2006 to January 2019), 2,446 TAVR procedures were performed at Cleveland Clinic, of which 2,032 (83%) were done using the transfemoral approach. Transfemoral TAVR increased over time as a percentage of TAVR procedures, while alternative approaches decreased.
Advertisement
Comparison of outcomes between the transfemoral approach and the collective alternative-access approaches showed similar rates of pacemaker requirements but showed the transfemoral approach to have lower rates of major vascular injury and higher rates of non-risk-adjusted five-year survival.
Among the alternative approaches, the vast majority of procedures involved transapical, transaortic or transaxillary access, with the favored alternative shifting from transapical to transaortic to transaxillary over time. Since 2016, transaxillary access has been the most common of all alternative approaches.
Analysis showed that compared with the intrathoracic approaches (transapical and transaortic), the transaxillary approach was associated with significantly fewer blood transfusions, lower rates of prolonged ventilation, less postoperative atrial fibrillation, shorter length of stay, greater likelihood of being discharged home and statistically similar rates of stroke.
“The transaxillary approach involves the least morbidity of all the alternatives to transfemoral TAVR,” says Dr. Yun.
Notably, propensity-matched comparisons of transfemoral versus transaxillary approaches since 2012 showed survival and major morbidity rates to be similar between the two methods. No brachial plexus injuries occurred in patients undergoing transaxillary TAVR.
“TAVR is evolving,” notes study co-author Samir Kapadia, MD, Chair of Cardiovascular Medicine at Cleveland Clinic. “Today’s devices and technology are more refined than in the past. In the early years, transapical access was the most common alternative for patients not amenable to transfemoral access. But now, at our center, transaxillary TAVR has become our preferred alternative TAVR approach.” He adds that the procedural shifts observed in this Cleveland Clinic study are consistent with national trends recently reported in the Transcatheter Valve Therapy registry.
Advertisement
“TAVR has grown in popularity year by year,” adds Dr. Yun, noting that TAVR volumes at Cleveland Clinic reached a new high of 732 in 2019, the first full year after completion of the study period reported here. “It is less invasive and frequently safer for frail older patients than surgical aortic valve replacement [SAVR].” While SAVR remains more common than TAVR at Cleveland Clinic, its volumes have declined modestly from a peak in 2010 as TAVR indications and volumes have expanded.
At Cleveland Clinic, decisions about a patient’s suitability for TAVR versus SAVR, as well as which TAVR approach to use, begin with a discussion by a multidisciplinary heart team. If TAVR is deemed the best choice, transfemoral access is the default. However, if the patient has small femoral or iliac arteries, significant calcification of these arteries or aorta, or severe aortic tortuosity, then transaxillary access is the next best option.
But not all these patients can undergo transaxillary TAVR:
Advertisement
“Cleveland Clinic is one of the few centers that offer alternative-access approaches,” notes interventional cardiologist Grant Reed, MD, MSc. “Our team-based approach allows us to guide every patient to the best treatment option, individualized for their specific situation. The close collaboration between cardiology and cardiothoracic surgery is one of the many reasons TAVR and SAVR outcomes are outstanding at Cleveland Clinic.”
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more