Non-fusion technique shows early promise

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Thousands of children undergo surgery for progressive scoliosis each year. Since the advent of modern medicine, the gold standard surgical technique is fusion of the involved vertebral elements. Over time, modern instrumentation has markedly improved our surgical techniques to improve our ability to realign and stabilize the spine. Until recently, surgery for scoliosis consisted of fusion almost exclusively, limiting spinal motion and creating additional stress on adjacent segments. Good long-term data exists showing success of this procedure.
Recently, newer techniques have been developed to permit guided growth for growing patients with progressive scoliosis. These techniques were developed to stabilize the spine and allow remaining growth to occur. During the post-surgical growth, the deformity can correct slowly over time.
This technique is similar to growth modulation techniques used in the lower extremities of children which have been commonplace for years. (i.e. stapling, physeal plating, epiphyseodesis). Vertebral body tethering is one such technique that permits continued growth without fusion and, as such, preserves motion.
As this is a relatively new procedure, indications continue to evolve. The procedure is designed to be performed in children with growth remaining and idiopathic curvatures between 35 and 70°. Children who are near skeletal maturity based on a bone age film or iliac crest apophysis are not candidates for this procedure. Goals of the procedure include stabilization of the convex portion of the curve with non-fusion instrumentation, modest correction in the operating room and completion of the deformity correction with future remaining growth.
Advertisement
The procedure is performed under general anesthesia in the lateral decubitus position with the convexity up, most typically the right side. Dual lumen endotracheal tube is preferred so that the lung can be collapsed for visualization. Standard neurologic monitoring is used in all cases. Video-assisted thoracoscopy is performed through four to five portals in the hemithorax.
Under camera visualization, as well as fluoroscopic guidance, anterior screws are placed in the vertebral bodies on the convexity along with a staple at each level. This instrumentation is then connected with a tether device that is flexible yet secures the instrumentation under tension which is controlled by the surgeon.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/722b75dd-3fa0-416c-ba67-cc04e7dbad3c/19-ORT-1446-Spine-CQD-Inset_jpg)
Intraoperative photo of video assisted thoracoscopy anterior vertebral body tethering.
Postoperative care typically consists of two to three days in hospital with a chest tube. Activity restrictions are in place for only six weeks, after which patients can resume all activities as tolerated. Patients are seen in follow-up at six-month intervals to monitor their radiographic changes as they grow. Complications are infrequent but it may include pulmonary complications, screw failure, tether failure, overcorrection and, rarely, neurologic injury.
As this technique is in its infancy, no long-term studies are yet available. Short to midterm data suggests the procedure is safe and can produce good correction both in the operating room and over time, eliminating the need for fusion. Future studies are warranted as the use of this technique becomes more widespread.
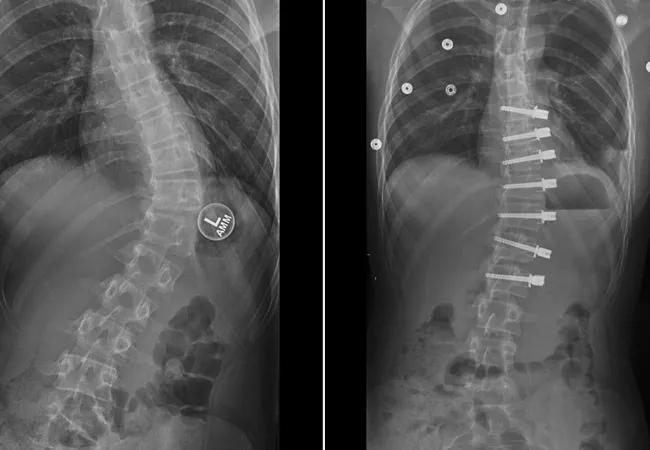
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/bece8749-01b0-4810-8919-f2863ae45c13/19-ORT-1446-Spine-CQD-Hero_jpg)
13-year-old female with progressive scoliosis treated with vertebral body tethering. Images show early correction from the preoperative posteroanterior x-ray and the patient’s first erect postoperative posteroanterior x-ray.
Dr. Goodwin is the Director of the Center for Pediatric and Adolescent Orthopaedics in the Orthopaedic & Rheumatologic Institute.
Advertisement
Advertisement

How it’s similar but different from the direct anterior approach

Collaboration must cross borders and disciplines

Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols

Should surgeons forgo posterior and lateral approaches?

How chiropractors can reduce unnecessary imaging, lower costs and ease the burden on primary care clinicians

Why shifting away from delayed repairs in high-risk athletes could prevent long-term instability and improve outcomes

Multidisciplinary care can make arthroplasty a safe option even for patients with low ejection fraction

Percutaneous stabilization can increase mobility without disrupting cancer treatment