Improved accuracy and fixation strength in spine surgery

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/032528ea-1f2f-4074-b984-9366ebe64310/17-ORT-1002-Gurd-Hero-Image-650x450pxl_jpg)
17-ORT-1002-Gurd-Hero-Image-650x450pxl
By Kyle Walker, MD, and David Gurd, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Pedicle screws are indicated for placement in procedures ranging from two-level vertebral fusions to complex spine reconstructions (i.e., idiopathic scoliosis). There are multiple methods to placing a pedicle screw, including a “freehand” method wherein a surgeon targets the trajectory of the screw blindly and/or aided by intraoperative fluoroscopy based on experience or with the aid of complex intraoperative navigation tools that typically require a large amount of radiation. Despite current best efforts, complications still occur given the proximity of the spinal pedicles to major anatomic structures, including the spinal cord, esophagus, lungs and aorta.
As an alternative approach to this complex surgical procedure, we investigated if outcomes could be improved with 3-D preoperative planning and patient-specific navigation (PSN) through use of a 3-D printed guide. Additionally, we sought to determine if fixation strength of pedicle screw placement could be improved through a computer algorithm that targets an optimized pedicle screw trajectory. The study was presented at the 2017 Scoliosis Research Society annual meeting and course.
Through use of 3-D reconstruction software, five cadaveric spines were virtually reconstructed and exported into a trajectory optimization software program for preoperative planning. One of two pedicles at each vertebral level from T1 to L5 was randomized to screw placement with either a PSN guide or through the freehand method, which served as a control. For the PSN-designated pedicles, an acceptable “start zone” was identified by a staff surgeon. Utilizing a proprietary algorithm, each pedicle screw trajectory was optimized within the bounds of this start zone.
Advertisement
Once the ideal trajectory was identified, a PSN guide was virtually generated with a canal aligned to the planned trajectory. A portion of each guide was designed to interface with the posterior lamina at the individual vertebral levels. The guides were then 3-D printed with a high-resolution, industrial printer with a material that can withstand high temperature and pressures, thus making it sterilizable for intraoperative use.
Figure 1 illustrates a virtual PSN guide aligned to the planned trajectory axis as well as the real-world screw that was placed aided by the 3-D printed guide.
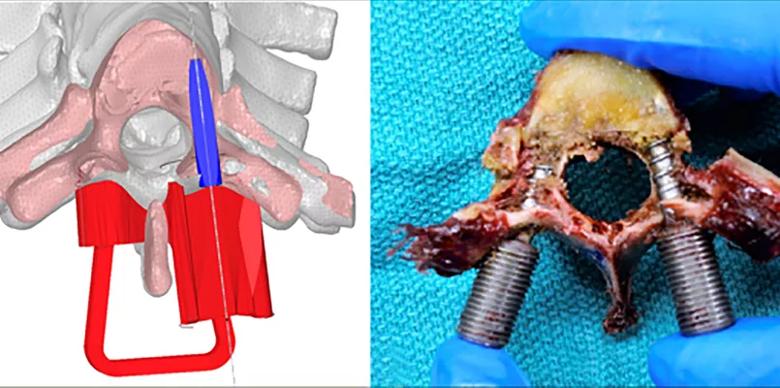
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3de65a3c-78a1-4a88-90f4-e922e0f2f30d/17-ORT-1002-Gurd-Inset-Image-805pxl-width_jpg)
Figure 1. Left image: Axial slice of the virtually planned trajectory with the PSN device (red) and a surrogate screw (blue) aligned to the trajectory axis. Right image: A similar axial cut in the real world vertebrae with the PSN screen on the right and the freehand-placed screw on the left.
The five cadavers previously described were assigned to five different surgeons of varying experience, ranging from intern to senior staff. Each surgeon was tasked with placing a freehand pedicle screw and a PSN-guided pedicle screw at each level without the aid of intraoperative imaging. After a pedicle screw was placed at each level, the cadavers were rescanned by way of computed tomography (CT) and virtually reconstructed. The postoperative CT scans were then compared for accuracy to the preoperatively planned trajectory. Across the five surgeons, accuracy of placement averaged less than 2.75 mm translation and 6.0 degrees angulation from the planned trajectory. Additionally, nearly half as many high-grade (grades 2 and 3) perforations were seen in the PSN-guided screws (13/84 versus 26/85).
Advertisement
In addition to an accurately placed screw, the average time to placement was over a minute faster for each screw placed using the PSN guide (136 +/- 80 seconds versus 201 +/- 82 seconds). This result is likely secondary to improved confidence during placement and less need for recheck for pedicle perforation during each step of the process. The total operative room time, however, would likely be improved even further upon this in a real world setting as the use of intraoperative fluoroscopy and/or neuromonitoring would inform the surgeon if a screw was grossly misplaced and required adjustment.
Each vertebral level was dissected and harvested in a way that allow axial load strength testing. Through use of the PSN guide and the optimization algorithm, the pedicle screws had, on average, 33.75 percent stronger fixation strength than the controls at each level. When looking at only the surgeons in this study that were postresidency, an average improvement in fixation strength of 28.6 percent was measured.
In this study, chosen screw size was controlled to avoid bias in either grouping, but the algorithm chose larger screws in over half of the PSN cases (31/59 biomechanically testable levels), which if used would have resulted in even stronger fixation at those levels.
Advances in 3-D reconstruction and printing technology have allowed the ability to create PSN guides that can conform to complex biological shapes. This technology can aid surgeons in rapid and accurate pedicle screw placement. Furthermore, coupling accurate placement with an optimization planning algorithm can improved fixation strength in even experienced surgeons. Moving forward, it will be important to test this technology in real world scenarios to investigate the clinical implications of these technologies and their ability to improve operative time, radiation exposure to the patient and surgeon, and rates of hardware failure.
Advertisement
Kyle Walker, MD, is a former Cleveland Clinic orthopaedic surgery researcher.
Advertisement
Advertisement
How it’s similar but different from the direct anterior approach
Collaboration must cross borders and disciplines
Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols
Should surgeons forgo posterior and lateral approaches?
How chiropractors can reduce unnecessary imaging, lower costs and ease the burden on primary care clinicians
Why shifting away from delayed repairs in high-risk athletes could prevent long-term instability and improve outcomes
Multidisciplinary care can make arthroplasty a safe option even for patients with low ejection fraction
Percutaneous stabilization can increase mobility without disrupting cancer treatment