Sarcoma Program shows we’re better together
By Lukas M. Nystrom, MD, and Nathan W. Mesko, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
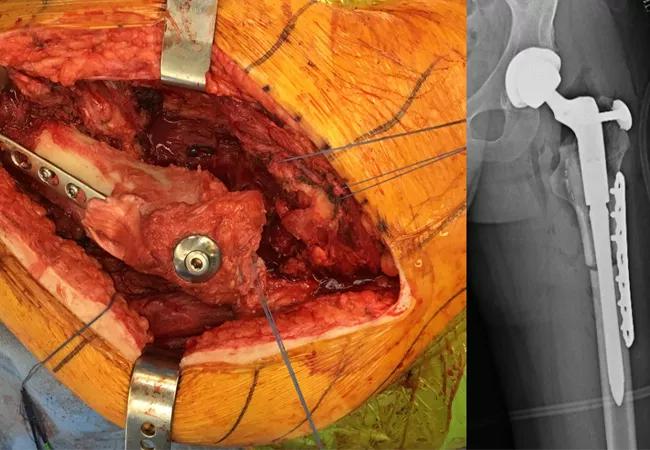
A young man in his early 20s presented to the Musculoskeletal Tumor Center with progressively worsening left hip pain. The patient had a history of a total hip replacement performed at another institution a year and a half prior to presentation for a pathologic femoral neck fracture (Figure 1). He had an uneventful recovery until July 2017, when walking became increasingly painful. Radiographs demonstrated an aggressive destructive mass surrounding his femoral implant (Figure 2) and pulmonary metastases (Figure 3). The mass was biopsied and confirmed to be a recurrent benign giant cell tumor of bone (Figure 4). His hip mass was treated with wide resection and reconstruction with an allograft-prosthetic composite (Figure 5). (Article continues below)

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/92c31bc5-db6c-462f-85a0-d8330c5b9a28/17-ORT-1244-Nystrom-Inset-01_650pxl-width_jpg)
Figure 1. Preoperative CT (left) demonstrating pathologic fracture through a radiolucent lesion in the left femoral head/neck extending to the level of the lesser trochanter; and postoperative radiograph (right) demonstrating reconstruction with a total hip arthroplasty.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3e3ffbec-b58a-40f3-acca-0f4c60c2a4db/17-ORT-1244-Nystrom-Inset-02_650pxl-width_jpg)
Figure 2. Left hip radiographs at the time of presentation demonstrating a large destructive mass around the left proximal femur.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/81ee73d7-295a-48bb-a30f-61603a046a55/17-ORT-1244-Nystrom-Inset-03_650pxl-width_jpg)
Figure 3. CT scan of the chest demonstrating one of multiple pulmonary nodules suggestive of metastases.
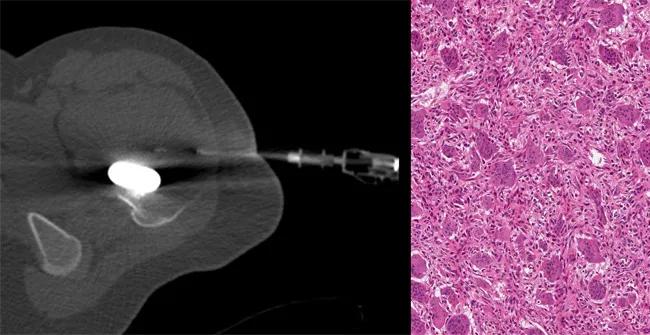
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/69ebbb0e-006e-4c3a-961e-405a640e1a13/17-ORT-1244-Nystrom-Inset-04_650pxl-width_jpg)
Figure 4. CT-guided core needle biopsy (left) of the mass performed by our musculoskeletal radiologist; tissue obtained from the biopsy was confirmed as giant cell tumor of bone (right).
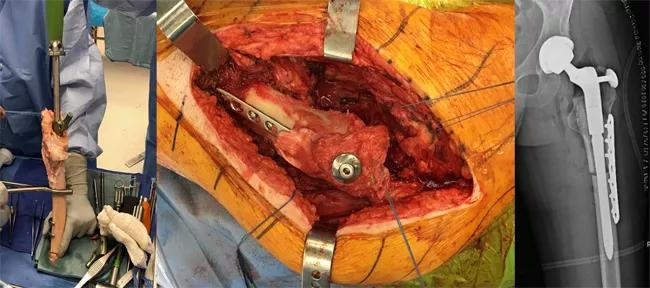
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b8507d73-b28d-4c48-b61c-4dafcfe33dac/17-ORT-1244-Nystrom-Inset-05_650pxl-width_jpg)
Figure 5. The allograft being prepared on the back table (left); the allograft-prosthetic composite implanted in the patient with supplementary bolt fixation and plate to resist rotation (center); postoperative radiograph (right) demonstrating reconstruction.
Advertisement
The successful care of this patient involved at least five medical specialties: radiology to interpret his multiple complex imaging evaluations and perform his image-guided biopsy, pathology to interpret biopsy results, medical oncology to discuss the pulmonary findings and develop a treatment plan, orthopaedic surgery to carry out the operation, and physical therapy to safely guide his rehabilitation.
Multidisciplinary care is imperative to providing high-quality care to patients with a musculoskeletal tumor diagnosis – which can range from malignant sarcomas, metastatic cancer involving muscle or bone, to complex benign aggressive tumors, such as the one described here.
Our comprehensive multidisciplinary Sarcoma Program allows us to better serve our patients by streamlining care across multiple disciplines, enabling us to diagnose and treat patients with great efficiency.
Our Sarcoma Program includes orthopaedic surgeons, other surgical subspecialists, medical oncologists (adult and pediatric), radiation oncologists, pathologists, radiologists, palliative medicine specialists, psychosocial oncologists and other practitioners. Each discipline plays a vital role in the care of the sarcoma patient.
Our multidisciplinary Sarcoma Tumor Board, which meets weekly, facilitates optimal communication and patient care. All core disciplines are present, and submit cases and contribute to the discussion. We discussed treatment options and came to a consensus at a tumor board meeting for the young man described above. The consensus was that in addition to treatment of the primary (hip) recurrent tumor location with wide resection, medical treatment with denosumab was needed for his pulmonary metastases.
Advertisement
An additional Sarcoma Program initiative involves developing specific care paths structured around certain bone and soft tissue sarcoma diagnoses. The care paths reflect our team’s agreement about how best to evaluate patients, structure timing of multidisciplinary treatments and determine frequency and type of disease surveillance patients should receive. Care paths help reduce unnecessary tests and decrease time to treatment as well as streamline processes in a way that is beneficial to patients and clinicians.
Sarcoma is a complex disease that requires a tremendous amount of very specialized expertise and care coordination. The only way to combat sarcoma and similar diseases is through collaboration across all medical specialties.
More about the Sarcoma Program:
Soft Tissue Sarcoma: The True Zebra You Don’t Want to Miss
Osteosarcoma: A Case Study in Why Multidisciplinary Collaboration Matters
Advertisement
Advertisement

How it’s similar but different from the direct anterior approach

Collaboration must cross borders and disciplines

Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols

Should surgeons forgo posterior and lateral approaches?

How chiropractors can reduce unnecessary imaging, lower costs and ease the burden on primary care clinicians

Why shifting away from delayed repairs in high-risk athletes could prevent long-term instability and improve outcomes

Multidisciplinary care can make arthroplasty a safe option even for patients with low ejection fraction

Percutaneous stabilization can increase mobility without disrupting cancer treatment