Recognizing and managing ocular syphilis and neurosyphilis
By Tamara A. Sussman, MD, Nabin K. Shrestha, MD, and Maria Miklowski, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 42-year-old man presented with intermittent fevers, rigors, headache and myalgia for six days, followed by blurred vision in his right eye with central vision loss for the past several hours. He reported no associated pain, flashes of light or floaters. He was sexually active with one male partner for 23 years. He had no history of human immunodeficiency virus (HIV), sexually transmitted infections or intravenous drug use.
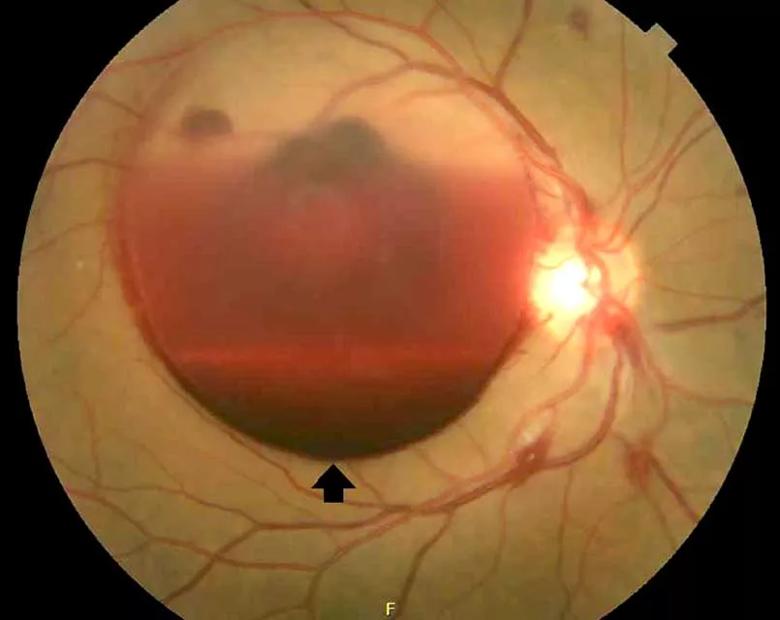
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/24b1f800-d7e4-4422-86c7-978320615f87/805x-Inset-1-sussman_ocularsyphilis_f1_jpg)
A dilated fundus photograph of the patient’s right eye shows large subhyaloid hemorrhage (arrow).
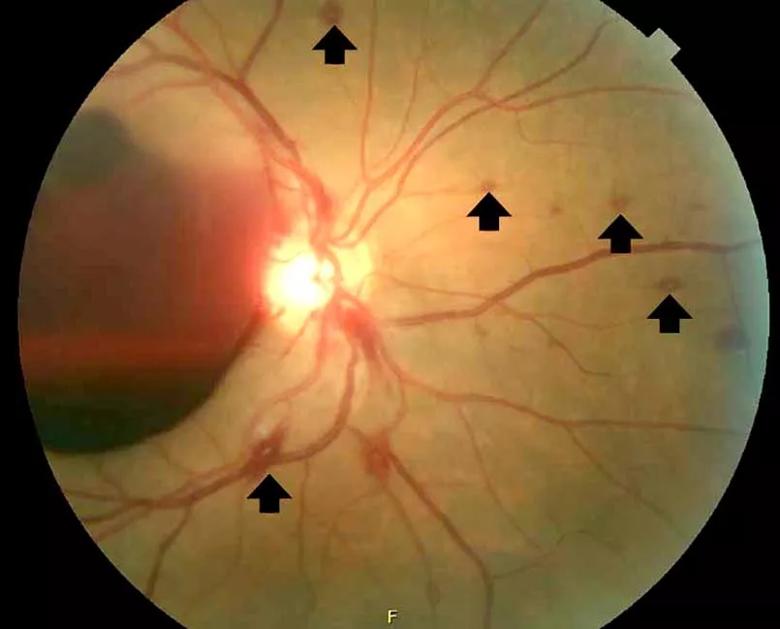
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/42a55c6a-a8f2-4be9-a55f-3d7120a25d14/805x-Inset-2-sussman_ocularsyphilis_f2_jpg)
Multiple white-centered intraretinal hemorrhages or Roth spots (arrows) were noted in the right eye.
Dilated funduscopy showed a large subhyaloid hemorrhage and retinal hemorrhages with white centers (Roth spots) in the right eye, and disc edema in the left eye.
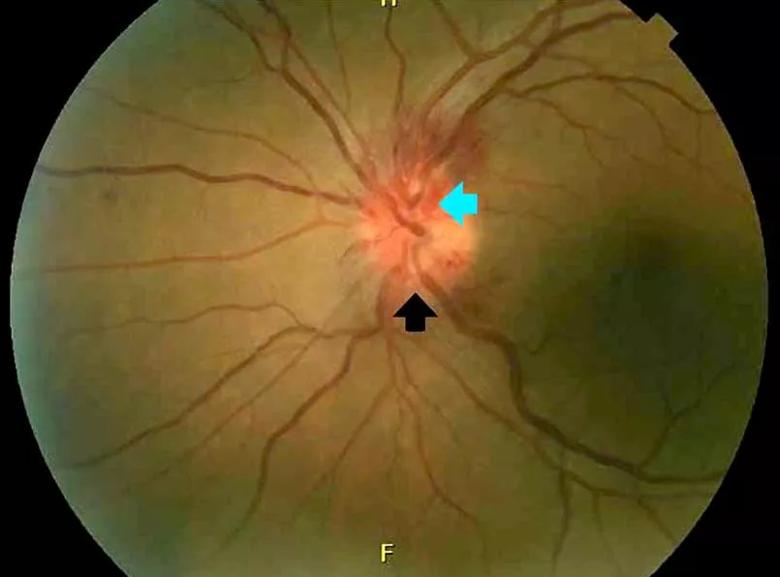
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a1efcad3-4e08-4f99-a070-af35b969bc02/805x-Inset-3-sussman_ocularsyphilis_f3_jpg)
A dilated fundus photograph of the left eye shows optic disc edema (black arrow) with associated optic disc hemorrhages (blue arrow).
On laboratory testing, serum rapid plasma reagin was reactive, Treponema pallidum immunoglobulin G was reactive (antibody index > 8.0) and HIV testing was negative.
Lumbar puncture study revealed 34 nucleated cells/µL (94 percent lymphocytes), protein 58 mg/dL and glucose 62 mg/dL. Cerebrospinal fluid Venereal Disease Research Laboratory and fluorescent treponemal antibody absorption tests were reactive, confirming a diagnosis of ocular syphilis.
The patient was admitted to the hospital for treatment with intravenous penicillin G. After five days, he was discharged with instructions to complete a 10-day course of intravenous ceftriaxone (chosen for its ease of administration), for a total of 14 days of antibiotic therapy. His vision improved with treatment.
Advertisement
He continued to follow up with ophthalmology and infectious disease. Subsequent dilated fundus examinations showed resolution of pathology in the left eye, resolution of Roth spots in the right eye and resolution of the subhyaloid hemorrhage. Repeat cerebrospinal fluid study examination was planned if the serum rapid plasma reagin had not become nonreactive 24 months after treatment.
In addition to ocular syphilis and neurosyphilis, the differential diagnosis for Roth spots and disc edema on dilated funduscopy includes endocarditis, viral retinitis and autoimmune or inflammatory conditions such as sarcoidosis and vasculitis.
In our patient, infectious endocarditis was considered, given his history of intermittent fevers and rigors, but it was ultimately ruled out by negative blood cultures and the absence of valvular vegetations on echocardiography.
The large subhyaloid hemorrhage raised suspicion of leukemia, but this was ruled out by the normal total white blood cell count and differential. HIV, herpetic retinitis and toxoplasmosis were also considered, but laboratory tests for these infections were negative.
Typically, retinal precipitates are more characteristic of syphilitic retinitis and distinguish it from other infectious causes such as herpetic retinitis and toxoplasmosis. Additionally, ocular syphilis more commonly manifests as uveitis or panuveitis. Our patient’s ocular syphilis presented with white-centered retinal hemorrhages, subhyaloid hemorrhage and optic disc edema.
Advertisement
About 90 percent of syphilis cases occur in men, and 81 percent occur in men who have sex with men. The US Centers for Disease Control and Prevention (CDC) thus recommends annual syphilis testing for men who have sex with men.
Classically, syphilis was called “the great imitator” because it mimicked manifestations of other diseases. Patients with ocular manifestations of syphilis may not have other neurologic symptoms. Nevertheless, cerebrospinal fluid examination should be done in all instances of ocular syphilis, as many patients with ocular syphilis have evidence of neurosyphilis on testing. The CDC also recommends follow-up cerebrospinal fluid analysis to assess treatment response. This was planned in our patient.
Dr. Sussman is an internal medicine resident. Dr. Shrestha is staff in the departments of Infectious Disease, Clinical Pathology and the International Travel Clinic. Dr. Miklowski is associate staff in Hospital Medicine.
This article was originally published in Cleveland Clinic Journal of Medicine.
Advertisement
Advertisement

Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma

Registry data highlight visual gains in patients with legal blindness

Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence

A look at emerging technology shaping retina surgery

A primer on MIGS methods and devices

7 keys to success for comprehensive ophthalmologists

Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs

Treatment options range from tetracycline injections to fat repositioning and cheek lift