Concomitant repair is a trade-off if tricuspid regurgitation is less than severe
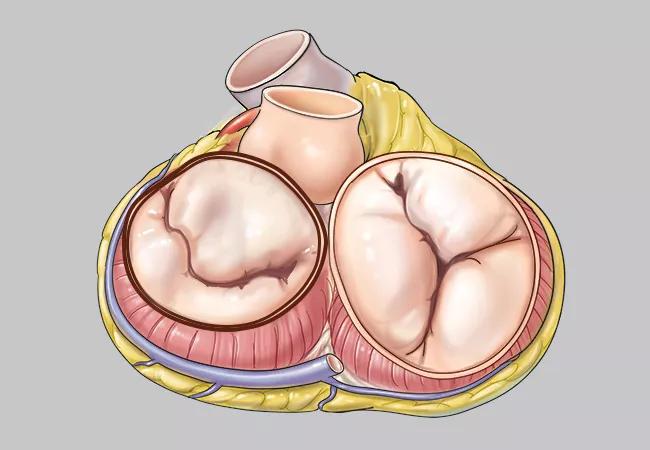
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5a1913fd-e9c7-429d-a6f7-8a410716e40f/22-HVI-2729215-CQD-650x450-1_jpg)
mitral and tricuspid heart valves in a medical illustration
Patients with degenerative mitral regurgitation (MR) and less than severe tricuspid regurgitation (TR) who undergo tricuspid annuloplasty along with mitral valve surgery are less likely to progress to severe TR than those who undergo mitral valve surgery alone. However, this benefit comes at the cost of a greater likelihood of permanent pacemaker implantation.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
So report investigators with the Cardiothoracic Surgical Trials Network (CTSN) after two years of follow-up of patients in a large international randomized trial. Study results were published in the New England Journal of Medicine (2022;386:327-339).
“Concomitant mitral and tricuspid valve surgeries in this population lowered the incidence of the study’s primary two-year composite endpoint, a result driven by reduced progression to severe tricuspid regurgitation,” says study co-author Marc Gillinov, MD, Chair of Thoracic and Cardiovascular Surgery at Cleveland Clinic, one of the trial sites. “However, combining the surgeries raised the risk of permanent pacemaker implantation more than fivefold. The jury is still out on the net clinical benefit of performing these procedures together in patients whose baseline tricuspid regurgitation is not severe.”
Although TR is common in patients undergoing mitral valve surgery for degenerative MR, how it should be managed is unclear. Evidence is strong that for patients with severe TR, concomitant repair of both valves confers overall benefit. Whether this is also the case for patients with lesser TR severity has not been established, however. “Current guidelines are based mainly on observational data from single centers,” says Dr. Gillinov, who serves as CTSN chair.
This uncertainty has led to wide variations in practice. The frequency of tricuspid valve repair at the time of mitral valve surgery ranges from 5% to 75%, the CTSN investigators note.
Advertisement
The study, conducted at 39 clinical sites in the U.S., Canada and Germany from 2016 through 2018, included 401 patients who were undergoing mitral valve surgery for degenerative MR and had either moderate TR or less than moderate TR with annular dilatation of at least 40 mm. Patients were randomly assigned to concomitantly undergo tricuspid annuloplasty or not. Evaluations were conducted regularly for two years. The study will continue to monitor patients annually for five years.
The primary endpoint at two years was a composite of the following: reoperation for TR, progression of TR by two grades from baseline or the presence of severe TR, or death.
At two years, patients in the tricuspid annuloplasty group had significantly fewer primary endpoint events (3.9% vs. 10.2%; relative risk = 0.37; 95% CI, 0.16-0.86). This advantage was driven primarily by a lower rate of TR progression, which was 0.6% in the tricuspid annuloplasty group versus 6.1% in the group that had mitral valve surgery alone. Risk of perioperative death was modestly but nonsignificantly lower in the tricuspid annuloplasty group. No reoperations were performed for TR in either group.
Major adverse cardiac and cerebrovascular events were similar between the study arms at two years, as were readmission rates, functional status and quality-of-life measures. However, conduction abnormalities were more frequent among those who underwent tricuspid annuloplasty, leading to a higher incidence of permanent pacemaker implantation (14.1% vs. 2.5%). Nearly 80% of implantations were performed during the index hospitalization.
Advertisement
Dr. Gillinov says the study provides strong evidence that concomitant tricuspid repair in patients undergoing surgery for degenerative MR is likely to provide benefit from slower progression of TR for at least two years — but at the cost of increased risk of needing a permanent pacemaker.
He identifies several further issues to consider:
“The full picture of long-term risks and benefits of tricuspid annuloplasty in this population has yet to be determined,” says Dr. Gillinov. “We hope to have some clearer answers when the five-year data are available.”
Advertisement
Advertisement
After four decades, refinements to the gold standard of bypass continue as new insights emerge
Why definitive surgical closure is the gold standard, and new ways to make it possible
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Cleveland Clinic’s new dedicated program offers nuanced care for a newly recognized cardiovascular risk factor
Scenarios where experience-based management nuance can matter most
Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics
How Cleveland Clinic is using and testing TMVR systems and approaches
NIH-funded comparative trial will complete enrollment soon