Also, earlier surgery likely benefits patients with severe functional TR
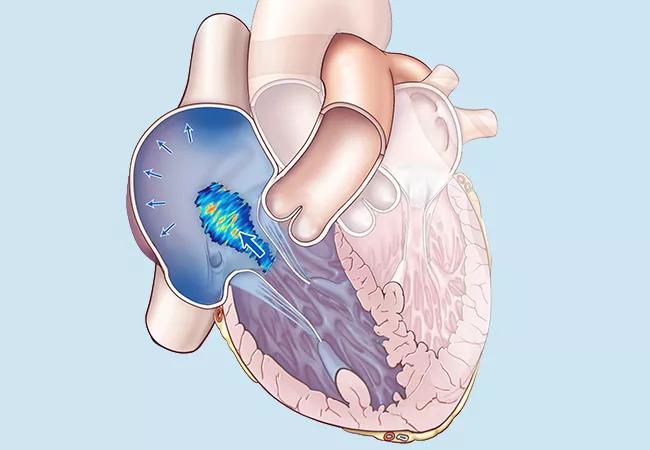
Good early outcomes of isolated tricuspid valve surgery for right heart failure support expanding surgical candidacy selection criteria. Additionally, patients with functional tricuspid regurgitation (TR) have poorer long-term outcomes than those with structural TR, which suggests they would benefit from earlier surgical intervention.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Those are two key conclusions of an observational study from Cleveland Clinic published online ahead of print in the Journal of Thoracic and Cardiovascular Surgery.
“Whether to operate on patients with severe tricuspid regurgitation and right heart failure is an increasingly common issue that cardiologists and cardiac surgeons struggle with,” says the study’s first author, Haytham Elgharably, MD, of Cleveland Clinic’s Department of Thoracic and Cardiovascular Surgery. “Our experience of good early outcomes following isolated tricuspid valve surgery supports expanding candidacy criteria, as well as operating earlier on patients with functional tricuspid regurgitation.”
He adds that the good early outcomes can be attributed to a thorough assessment process for these patients before surgery, which may include cardiac MRI in addition to routine testing such as echocardiography and right/left cardiac catheterization. The evaluation is then completed by direct discussion among Cleveland Clinic’s right heart failure team, including both cardiology and cardiac surgery, to carefully select candidates for surgery. “In our experience,” Dr. Elgharably says, “two critical factors of risk assessment should be considered when planning for surgery: right ventricular function and the liver function profile. High-risk patients are evaluated for available transcatheter therapies.”
No standard approach exists for determining operability and likelihood of reversing right heart failure in patients with tricuspid valve disease, with a variety of clinical factors entering the equation.
Advertisement
Most would agree that surgery is indicated for those with normal right ventricular function and cardiac index and mild right heart failure, as such patients are generally low risk and tricuspid valve surgery is likely to achieve successful reversal.
On the other end of the spectrum, the decision not to operate is relatively easy for those with right ventricular dysfunction, low cardiac index and severe right heart failure, as such patients are at high surgical risk and reversal of heart failure is unlikely.
Not so clear-cut, however, is what to do in settings between these extremes — i.e., in patients with normal right ventricular function and normal cardiac index but severe right failure, or in those with right ventricular dysfunction, low cardiac index and only mild right heart failure.
The Cleveland Clinic researchers’ new observational study was designed to characterize patients with right heart failure who underwent isolated tricuspid valve surgery to better identify criteria for candidacy.
The study included 62 patients who underwent isolated tricuspid valve surgery at Cleveland Clinic from 2007 to 2014. Patients had severe, long-standing tricuspid valve disease and variable degrees of right heart failure and liver dysfunction. Mean age was 57 ± 16 years, and 60% of patients were women. Nearly three-quarters of patients (n = 45) had undergone at least one previous heart operation, including 19 surgeries on the tricuspid valve (10 repairs, nine replacements).
Hospital outcomes included reoperation for valve dysfunction (3.2%), renal failure (4.8%) and one death (1.6%) for a respiratory-related complication.
Advertisement
Cluster analysis was conducted of right heart morphology and function variables from stored echocardiographic images and clinical and hemodynamic data from patient records.
Tricuspid valve variables split patients into two equal clusters: those with functional TR and those with structural TR. Relative to patients with structural TR, those with functional TR had the following characteristics:
“Despite worse heart failure among patients in the functional TR group, their right ventricular function was similar to that of patients with structural TR,” Dr. Elgharably comments. Cluster analysis also revealed that right ventricular size was more predictive of right heart failure than right ventricular function was.
“Patients with severe tricuspid regurgitation and right heart failure have often been considered too high risk and denied surgery as a result,” notes study co-author Patrick Collier, MD, PhD, a cardiologist in Cleveland Clinic’s Section of Cardiovascular Imaging. “This study demonstrates good early surgical outcomes for many of these sick patients and supports referral of such patients by cardiologists. It also shows that careful patient selection is key to better defining of operability and the risks and benefits of tricuspid valve surgery.”
Advertisement
The authors draw two major conclusions from this study:
“Liberalizing criteria should be considered in carefully selected patients,” Dr. Elgharably says, “Findings indicate that patients are likely to have good short- and intermediate-term outcomes, although their long-term prognosis is uncertain.”
Advertisement
He adds that the mortality rate in this study was considerably lower than what is reported in the literature, which typically runs from 8% to 20%. He attributes this in part to careful patient selection, with special attention to ensuring adequacy of right ventricular function and liver function.
Advertisement

Scenarios where experience-based management nuance can matter most

Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients