Researchers urge caution when managing AAA in this population
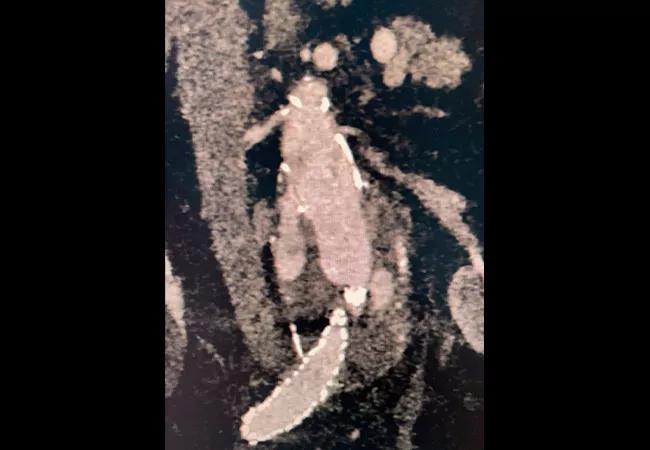
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ee2da36a-b17a-48ba-a423-cf231166e83c/21-HVI-2246258_aortic-aneurysm-with-wide-neck_650x450_jpg)
21-HVI-2246258_aortic-aneurysm-with-wide-neck_650x450
A wide proximal aortic neck appears to put patients at greater risk for complications and death following endovascular aneurysm repair (EVAR) for treatment of abdominal aortic aneurysm (AAA). According to a systematic literature review and meta-analysis by Cleveland Clinic researchers, the incidence of major adverse events such as endograft migration and endoleakage with EVAR is significantly higher in patients with large-diameter infrarenal necks than in those with normal aortic necks.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Recently published in the Journal of Vascular Surgery(2021;74:309-315), the analysis evaluated the outcomes of 7,448 patients who were treated for AAA with EVAR across 11 published trials that met the study’s inclusion criteria, which were based on PRISMA standards. The median age of subjects was between 72.7 and 76.5 years; 89.1% were male. Follow-up ranged from 2 to 5 years.
Of the 7,448 patients, 26.9% were classified as having “wide” aortic necks, defined as a diameter between 25 mm and 30 mm or greater. Weighted averages of composite major adverse events and aneurysm-related mortality were greater in the group with wide aortic necks (33.5% and 15.3%, respectively) than in the cohort with normal diameters (21.2% and 3.9%, respectively).
“Thanks to technological advances and improved device instructions, neck anatomy poses fewer restrictions than it once did, but these breakthroughs have prompted some clinicians to push the limits of EVAR by using the procedure to manage patients with ectatic or wide aortic necks,” explains Cleveland Clinic vascular surgeon Francis J. Caputo, MD, who conducted the meta-analysis with vascular surgery resident David J. Laczynski, MD. “Unfortunately, evidence suggests that such patients suffer from a higher incidence of proximal neck degeneration, reintervention, and morbidity and mortality.”
The meta-analysis also revealed that the risks of aneurysm rupture and aneurysm sac enlargement were higher in those with wide aortic necks. Type I and Ia endoleaks, which are frequently caused by insufficient sealing at the graft attachment site, were more common in patients with wide aortic necks than in those with normal diameters (11.3% vs 3.1%; P < 0.001). There was no difference in the rate of type Ib endoleaks between the two cohorts.
Advertisement
EVAR has surpassed open surgery as the principal treatment for AAAs in patients with appropriate anatomy; however, the procedure is limited by its inability to achieve a sufficient seal between the endograft and aortic wall. One study in the meta-analysis, which noted an increase in proximal fixation failure in patients treated with large-diameter devices, recommended the use of proximal seal strategies with fenestrated or branched devices when managing patients with wide aortic necks. Although there were no reported endograft fractures in patients with wide aortic necks, endograft migration at 5 years was higher in this population.
“EVAR remains an option for patients with wide aortic necks, particularly when open repair is unfeasible, but close long-term surveillance is paramount to stem the potentially catastrophic complications seen in this high-risk population,” cautions Dr. Caputo. “There are a variety of factors that must be considered when initiating EVAR, including device selection and instructions for use, but studies confirm that neck diameter is among the most important predictors of success when using this procedure to manage patients with AAA.”
The study authors highlight one particularly important limitation of their research: the lack of consensus on what constitutes a “wide” aortic neck, which they note their analysis underscores. They call for agreement on a standard definition for wide-neck aneurysms, an argument echoed by an invited commentary accompanying their study by two vascular surgeons at the University of Alabama at Birmingham.
Advertisement
“Given mounting evidence regarding the impact of neck diameter, we feel that the lack of consensus on this definition should be addressed and recommendations incorporated into practice guidelines,” the editorialists write, adding that variability in neck size based on patient stature and body mass index should also be taken into account.
Advertisement
Advertisement
After four decades, refinements to the gold standard of bypass continue as new insights emerge
Why definitive surgical closure is the gold standard, and new ways to make it possible
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Cleveland Clinic’s new dedicated program offers nuanced care for a newly recognized cardiovascular risk factor
Scenarios where experience-based management nuance can matter most
Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics
How Cleveland Clinic is using and testing TMVR systems and approaches
NIH-funded comparative trial will complete enrollment soon