JACC State-of-the-Art Review features care algorithm and more
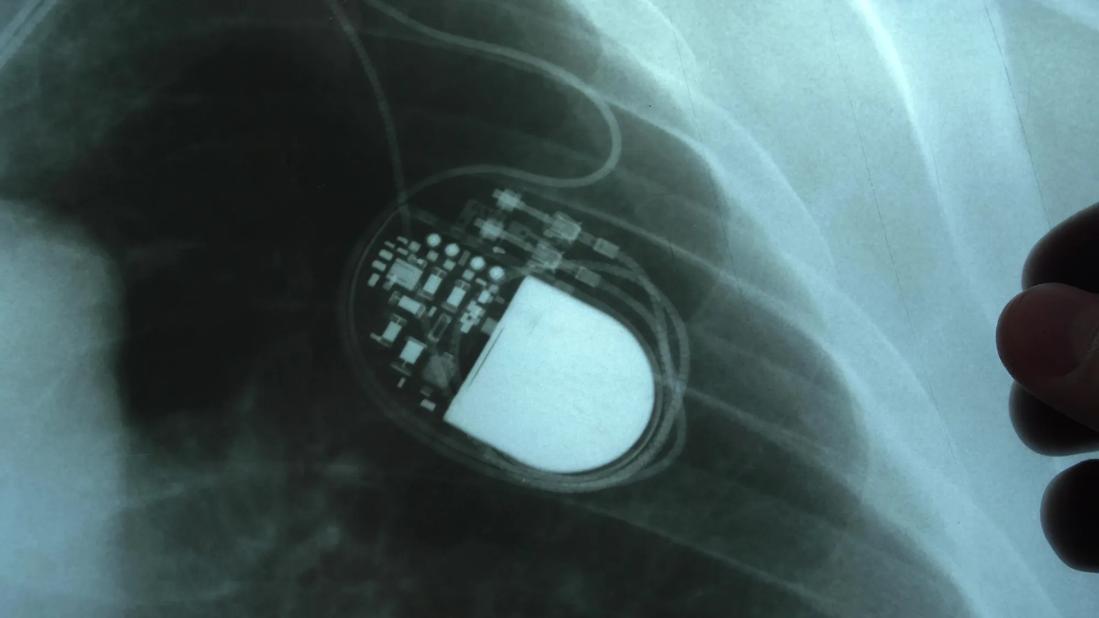
The emergence of transcatheter aortic valve replacement (TAVR) as an alternative to surgery for patients with severe aortic stenosis has been universally welcomed, but it doesn’t come without caveats. A leading one is the heightened post-procedural risk of advanced conduction abnormalities, most notably new-onset left bundle branch block (LBBB) and high-grade atrioventricular block (AVB) requiring implantation of a permanent pacemaker (PPM).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The fast-evolving landscape around PPM requirements in TAVR patients is the focus of a helpful new “State-of-the-Art Review” in JACC: Cardiovascular Interventions (2021;14:115-134) by a group of authors predominantly from Cleveland Clinic.
“Despite ongoing improvements in TAVR safety and efficacy, conduction abnormalities that require PPM placement remain a common development following TAVR because of the proximity of the atrioventricular conduction system to the aortic root,” explains the review’s senior and corresponding author, Samir Kapadia, MD, Chair of Cardiovascular Medicine at Cleveland Clinic. “As TAVR use expands in the wake of its August 2019 FDA approval for patients at low surgical risk, there is increased need to understand the impact of both PPM implantation and post-TAVR conduction abnormalities on mortality and other outcomes.”
To promote that understanding, Dr. Kapadia and colleagues performed a systematic literature search through mid-2020 for comprehensive data on the following:
Their resulting review outlines and interprets current evidence on these issues, presenting data across a number of reader-friendly tables, figures and illustrations. The latter include a central illustration presenting Cleveland Clinic’s algorithm for managing conduction disturbances and assessing need for PPM placement after TAVR. “We offer our rationale for atrial pacing in the immediate post-TAVR environment to further risk-stratify patients in terms of PPM requirement,” Dr. Kapadia explains.
Advertisement
Across the course of the review, the authors share a number of conclusions, including the following:
“We also urge heart teams to carefully consider specific anatomic, electrical and clinical risk factors when evaluating candidates for TAVR,” Dr. Kapadia notes. “Moreover, clinicians’ choice of valve and implantation technique should be made with an aim to minimize the risk of post-procedural conduction abnormalities. The duration and need for post-procedural monitoring of heart rhythm prior to committing the patient to a permanent pacemaker is something that needs further investigation.”
The full State-of-the-Art Review is available here.
Advertisement
Advertisement

Patient series and bench validation support efficacy and safety of CLEVE procedure

For many patients, repair is feasible, durable and preferred over replacement

In experienced hands, up to 95% of patients can be free of reoperation at 15 years

Multidisciplinary teams can deliver good short- and long-term outcomes, Cleveland Clinic experience shows

Experience and strength in both SAVR and TAVR make for the best patient options and outcomes

Ideal protocols feature frequent monitoring, high-quality imaging and a team approach

Age and other factors figure into the choice among SAVR, TAVR, Ross, Ozaki and more

Optimally timed valve replacement depends on an expert approach to nuanced presentations