Orthopaedic surgeon discusses an innovative robotic technique for total hip arthroplasty

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Robotic-arm assisted total hip arthroplasty (THA) is an exciting technology that can benefit patients for routine and complex cases alike. The system (Mako, Stryker Orthopaedics) is compatible with all common hip approaches, and can be incorporated into a busy adult reconstruction practice.
Potential advantages include:
In a recent clinical case, a 67-year-old female presented with complaints of severe pain and grinding in her right hip, inability to ambulate and shortening of the leg. She had no significant past medical history aside from being a current smoker. She had received a corticosteroid injection three months previously for treatment of hip osteoarthritis. Prior radiograph before the injection (Figure 1) shows severe hip osteoarthritis and current radiograph (Figure 2) indicates rapidly progressive arthritis with joint destruction, severe acetabular and femoral bone loss. Preoperative aspiration was negative for infection. She was indicated for complex primary THA, and was counselled preoperatively about smoking cessation. Given the complexity of the acetabular reconstruction, I elected to do the case with robotic assistance to allow for accurate bone preparation and implant placement.
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6089657c-d58b-4c25-967e-688454526436/19-ORT-1448-Robotic-Hip-CQD-Inset-1-2_jpg)
A preoperative CT scan was obtained and the reconstruction was planned using the software. After choosing the desired inclination and version, the acetabular component is sized and placement is chosen in all three planes relative to the host bone, in quarter-millimeter increments. I planned the reconstruction near the native hip center, which allowed for fit between the remaining anterior and posterior walls (Figure 3). There was a large segmental acetabular defect of the superior dome with uncoverage of the implant (Figure 4), and a superior acetabular augment was planned. After planning the femoral reconstruction, the approximate leg length and offset are restored.
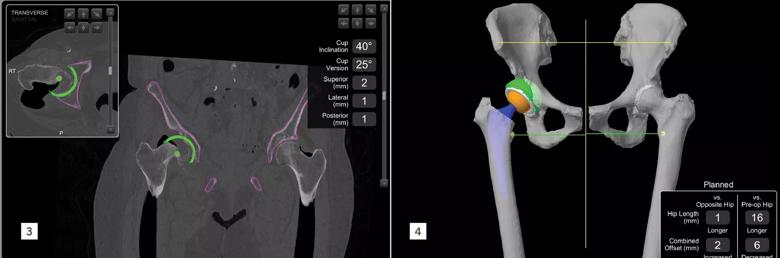
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e475c79c-48a5-46ee-993a-1d633750d6ef/19-ORT-1448-Robotic-Hip-CQD-Inset-3-4_jpg)
This case was done through a posterior approach, and wide acetabular exposure around the defect was accomplished. The acetabular bone was registered with the optical navigation, and the registration was verified to ensure accuracy (Figure 5). The robotic arm was then brought in, and used to ream the bone according to the preoperative plan. With good bone preparation, the final implant was inserted with the robotic arm locking the impactor into the chosen orientation. A multihole revision cup was used in this case for enhanced screw options. Although the cup was significantly uncovered superiorly as expected, the press-fit between the walls was very good, and four screws were placed into the remaining acetabular bone to augment initial fixation. We trialed and selected a superior acetabular augment which was then fixed to the pelvis with three additional screws. The construct was unitized by placing cement between the augment and cup, and a dual mobility articulation was chosen for elevated risk of instability. The femur was broached and the hip trialed, with excellent stability and recreation of clinically equal leg lengths. After placement of the final implants, the leg length and offset were verified using the computer. At the most recent follow-up three months postoperatively, radiographs (Figure 6) show the final reconstruction, and the patient was recovering appropriately with no hip pain.
Advertisement
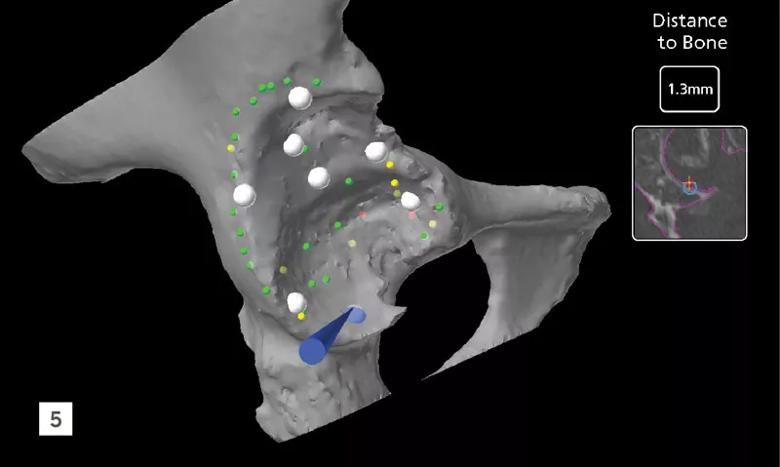
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/30b8b3b8-39a2-4086-a9e9-1d28a06a01eb/19-ORT-1448-Robotic-Hip-CQD-Inset-5_jpg)
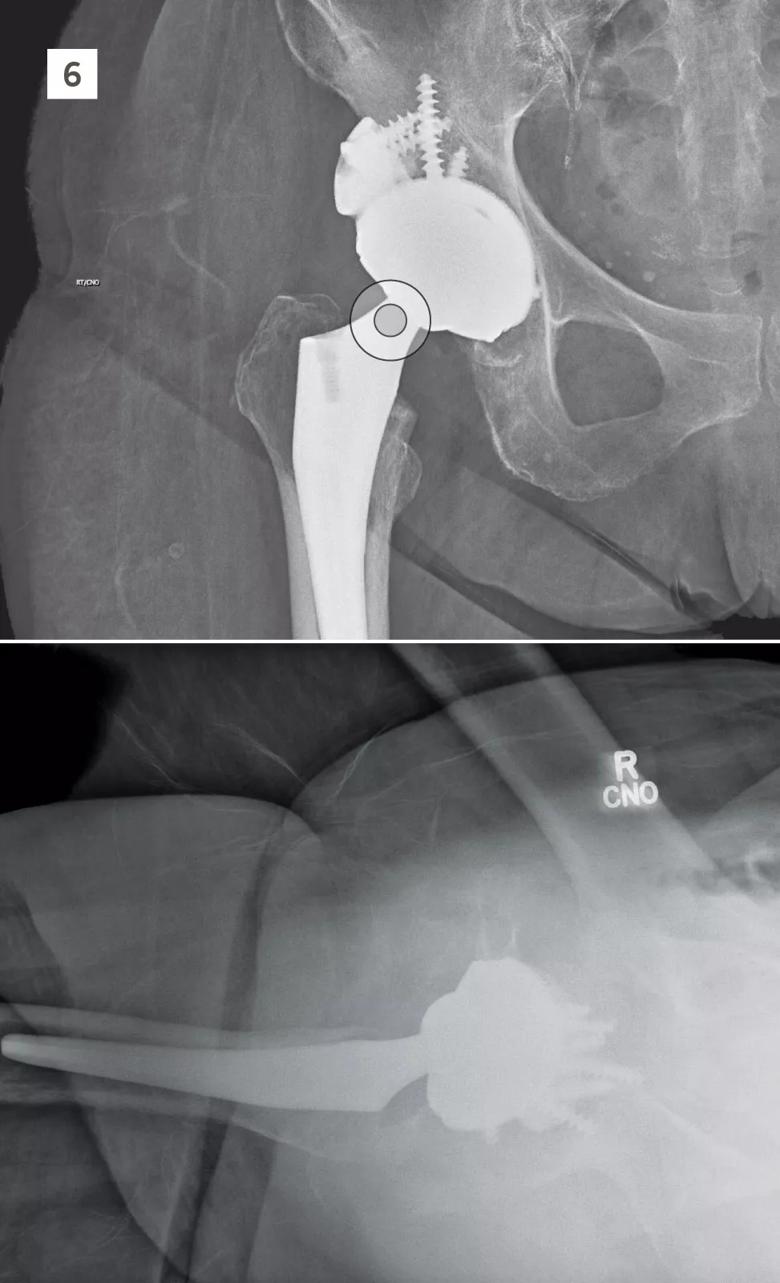
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/fe6af835-0c25-4927-9c89-6ce0555cd2d4/19-ORT-1448-Robotic-Hip-CQD-Inset-6_jpg)
Dr. Bloomfield is a board-certified orthopaedic surgeon subspecializing in adult reconstruction. His interests include robotic-assisted hip and knee arthroplasty, as well as complex primary and revision joint replacement. For inquiries, please call 440-312-0710.
Advertisement
Advertisement

How it’s similar but different from the direct anterior approach

Collaboration must cross borders and disciplines

Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols

Should surgeons forgo posterior and lateral approaches?

How chiropractors can reduce unnecessary imaging, lower costs and ease the burden on primary care clinicians

Why shifting away from delayed repairs in high-risk athletes could prevent long-term instability and improve outcomes

Multidisciplinary care can make arthroplasty a safe option even for patients with low ejection fraction

Percutaneous stabilization can increase mobility without disrupting cancer treatment