Both manual and semi-automated CTA methods can be highly reliable, study shows
Two CT angiography (CTA) methods of measuring the maximum diameter (Dmax) of an abdominal aortic aneurysm (AAA) — multiplanar reformations based on orthogonal planes and semi-automated centerline flow analysis — can result in similar values as well as high concordance between readers. So concludes a Cleveland Clinic study conducted using standardized measurement protocols, recently published online in Annals of Vascular Surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The Dmax of an aneurysm is one of the most important factors determining a patient’s clinical course, and even small differences in values can have significant impact,” says senior author Francis Caputo, MD, a Cleveland Clinic vascular surgeon. “It’s critical that measurements are accurate and reproducible among different methods and by different readers of the images.”
For patients with an AAA, when to intervene is based largely on Dmax. A variety of methods exist for obtaining this measure, but there is neither a consensus on which method is best nor standardized protocols for conducting measurements. This can lead to potentially clinically significant variability in values, depending on the reader and the method used.
Although ultrasonography is widely available and entails no radiation for measuring Dmax, it is less accurate than CTA.
Earlier studies used axial, coronal and sagittal slices to obtain Dmax, and axial measurements were once favored as the gold standard. “These methods are now deemed inadequate, however, because of significant intra- and interobserver variability and the fact that they may not accurately capture true dimensions in tortuous vessels,” says study co-author and Cleveland Clinic vascular surgeon Jarrad Rowse, MD.
Currently, two CTA methods of measuring Dmax are commonly used:
Advertisement
The recent Cleveland Clinic study was designed to evaluate accuracy and reproducibility of results obtained with these two CTA methods.
A retrospective chart review was conducted of adult patients with an AAA (maximum diameter in any direction > 35 mm) who had been followed by CTA at Cleveland Clinic during 2019.
Dmax was measured using existing pre-intervention images (using multiplanar reformations based on orthogonal planes and semi-automated centerline analysis; see Figures 1 and 2) by a vascular surgeon, a radiologist and an imaging cardiologist. Each reader used a standardized protocol for obtaining Dmax with both methods and repeated the process after several weeks to evaluate intraobserver consistency.
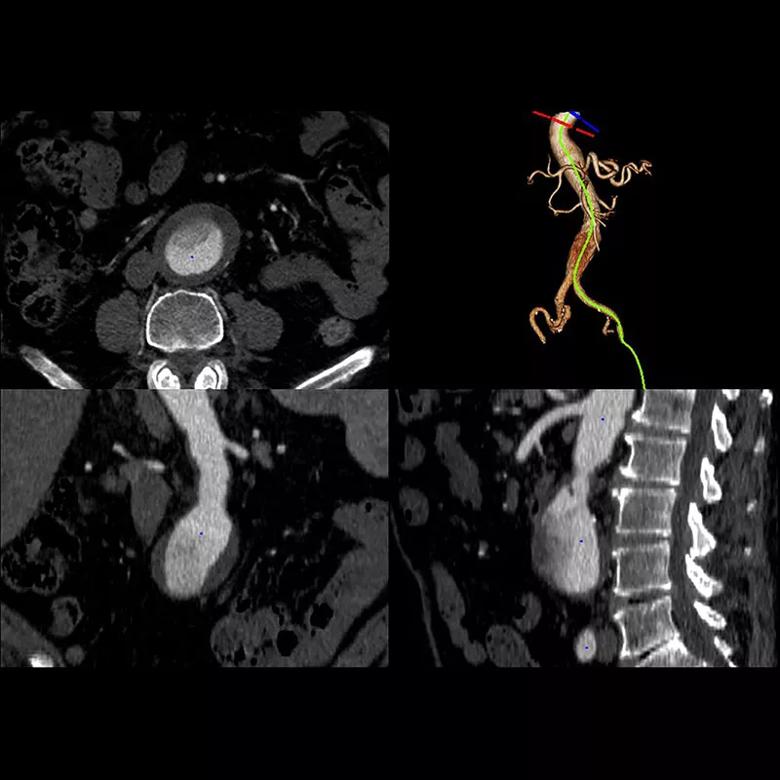
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b9ea14db-db6d-4657-bf85-d94864e44671/21-HVI-2541216-CQD-Inset-1-800x800-1_jpg)
Figure 1. Multiplanar reformation of an abdominal aortic aneurysm.
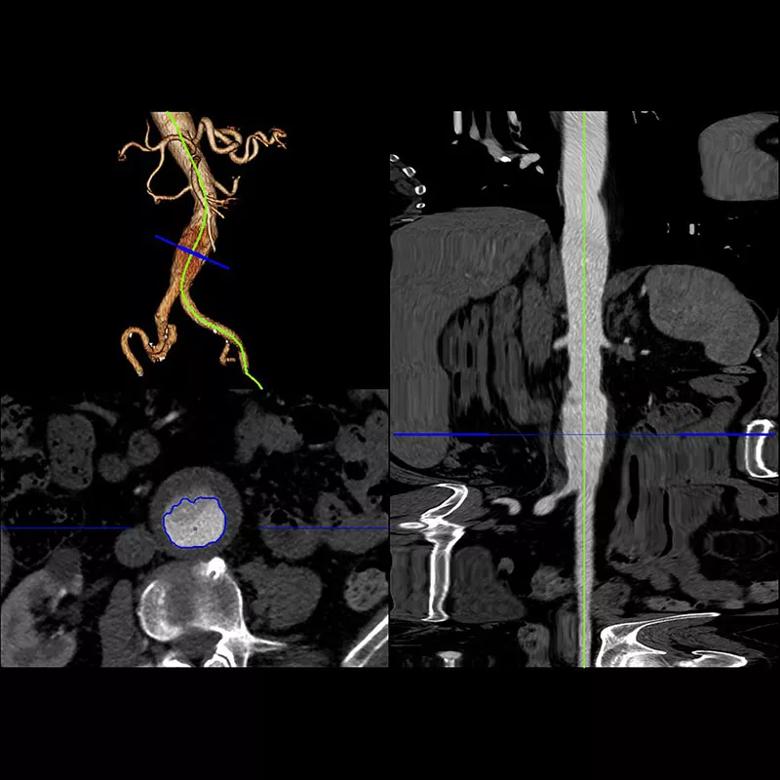
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/bf48030b-5e20-40ca-9566-99644d104a6a/21-HVI-2541216-CQD-Inset-2-800x800-1_jpg)
Figure 2. 3D volume rendering showing straightening of the aorta to provide the centerline.
Obtained values were also compared with the original radiology reports from Cleveland Clinic or outside hospitals.
Various statistical methods were employed to analyze inter- and intraobserver results, evaluate concordances between the different methods, and compare obtained values with the original clinical reports. A 3-mm threshold was used to define concordance.
Mean age of the cohort was 75 years (range, 47-90); 81% of patients were male, and more than 90% were white. Dmax was measured in 148 AAAs, with diameters ranging from 3.8 to 9.6 cm.
The protocolized methods resulted in high agreement, as follows:
Advertisement
Notably, the differences in concordance were not statistically significant between readers nor between methods, and no discordances were greater than 5 mm.
In the original radiology reports, Dmax was measured using axial, sagittal and coronal imaging. The following concordance rates were observed:
The authors stress the following points from this study:
Advertisement
“This study underscores opportunities in precise measurement of aortic dimensions in patients with thoracoabdominal aortic aneurysms,” observes cardiovascular imaging specialist Milind Desai, MD, MBA, Director of Clinical Operations in Cleveland Clinic’s Heart, Vascular & Thoracic Institute, who was not involved in the study. “It highlights the importance of orthogonal reconstruction of the 3D dataset for reproducible measurements by experienced imagers.”
“Accurate and reproducible methods for measuring Dmax should be obtainable with recent advancements in CTA imaging and post-processing methods,” Dr. Caputo concludes. “Standardization of obtaining Dmax and providing defined measurements are paramount within and between institutions.”
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more