Aortoiliac stenting with bifurcation reconstruction compares well with aortobifemoral bypass
For patients with severe aortoiliac occlusive disease, aortoiliac stenting with bifurcation reconstruction (AISBR) is increasingly used to avoid open surgery with aortobifemoral bypass (ABF). A new study finds that this less-invasive approach is associated with reductions in blood loss, hospital length of stay and surgical site infections compared with the traditional ABF option.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The findings are from a single-center retrospective investigation of both strategies performed at Cleveland Clinic to treat Trans-Atlantic Inter-Society Consensus Document (TASC II) lesions class D (infra-renal aortoiliac occlusion) in comparable patients. The study was published online in Annals of Vascular Surgery.
“Complex total or hybrid endovascular management of TASC II D aortoiliac occlusive disease has largely supplanted traditional open aortobifemoral bypass at Cleveland Clinic, especially for patients at elevated surgical risk,” says study co-author Sean Lyden, MD, Chair of Cleveland Clinic’s Department of Vascular Surgery. “This review of our experience over nearly a decade reassures us that it offers reduced morbidity and acceptable outcomes.”
Open surgery with ABF is the traditional treatment for severe aortoiliac occlusive disease, but because it requires laparotomy and aortic manipulation, along with bilateral femoral artery exposure, many patients are poor candidates. To extend treatment to marginal and high-risk operative patients, AISBR — involving complex endovascular reconstruction of the infrarenal aorta and iliac arteries — has become increasingly popular. However, data comparing the two treatment strategies are scarce.
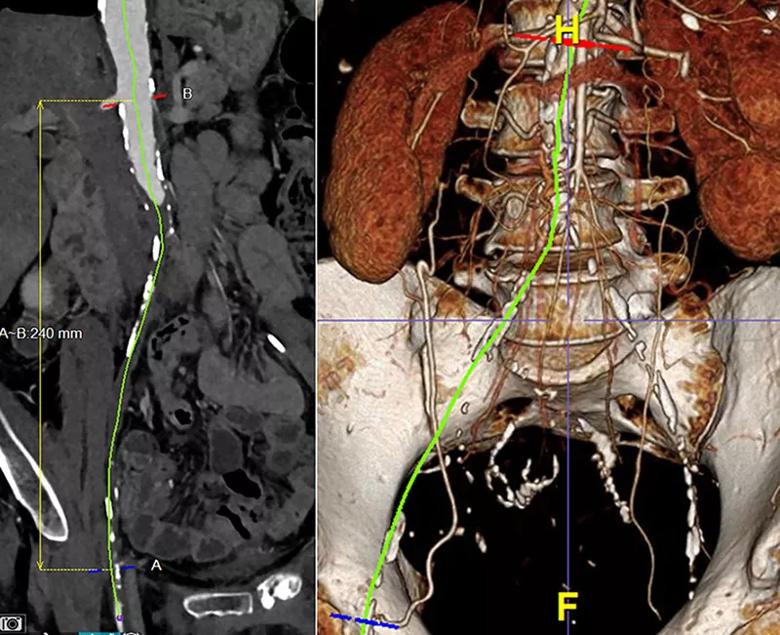
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/19449620-9c77-4b27-8e56-787880b351dc/21-HVI-2588340-CQD-Inset-800x650-1_jpg)
Reformatted images (centerline reconstruction on the right and 3D reconstruction on the left) of a CT angiogram of a patient with TASC II D aortoiliac occlusive disease — in this case a distal aortic occlusion and bilateral iliac artery occlusions. Using high-quality imaging and reprocessing software to create these images helped in treatment planning for this patient, who went on to receive endovascular recanalization of these aortoiliac occlusions.
Advertisement
The study included patients who underwent AISBR (n = 75) or ABF (n = 24) for TASC II D disease at Cleveland Clinic between 2010 and 2018. To increase comparability between cohorts, all ABF patients were those deemed candidates for AISBR based on review of preoperative imaging.
The primary indication for treatment was claudication (56% of patients), followed by rest pain (28%) and tissue loss (16%).
Femoral endarterectomies were performed in 49% of AISBR cases and 58% of ABF cases (difference not significant).
A wide variety of endovascular devices were used in the AISBR procedures, but most had uncovered stents in the infrarenal aorta and common/external iliac arteries. Procedural outcomes of AISBR were as follows:
At five-year follow-up, there was no significant difference between the groups in primary assisted patency, secondary patency, freedom from re-intervention, or major adverse limb events. Survival was 76.5% for AISBR vs. 100% for ABF (P = 0.07).
The researchers emphasize that at least two points should be considered when interpreting these findings:
1) Lower survival numbers with AISBR probably reflect bias. The trend in different survival rates between the procedures likely reflects selection bias, according to Dr. Lyden. “We are using AISBR in most patients now, but historically we had reserved this less-invasive approach for sicker patients with multiple comorbid conditions while employing ABF for those who were younger and fitter.”
Advertisement
2) For many patients, the potential for a lower primary patency rate with AISBR is tempered by other factors. One factor is the learning curve of complex endovascular recanalizations and reconstructions. Additionally, considering the reduced hospital stay, blood loss and surgical-site infection risk associated with AISBR, “many doctors and their patients would likely prefer the possibility of needing a second percutaneous procedure in the future over undergoing a large, open aortic reconstruction,” Dr. Lyden notes.
The researchers note that comparative studies between AISBR and ABF are rare, and that such investigations face multiple obstacles. Creating comparable cohorts is a challenge because of the heterogeneity in patient anatomy; this study used preoperative imaging to confirm candidacy for both procedures to mitigate this problem. “Furthermore, there is a historical bias toward and dogma associated with ABF,” Dr. Lyden says.
Comparisons are also made difficult by the variety of endovascular reconstruction techniques and stent choices available. Cleveland Clinic surgeons use several methods of AISBR, including unibody, bifurcated stent-grafts and trimodular stenting of the infrarenal aorta and bilateral common iliac artery. Bare metal iliac stents are preferred for AISBR at the institution.
According to the authors, future studies are needed to help sort out optimal devices and configurations to manage aortoiliac occlusive disease and to identify anatomic factors that may favor one strategy over another. Patency rates beyond five years also need investigation.
Advertisement
“In the meantime, outcomes from this study provide support that AISBR is a reasonable alternative to ABF,” Dr. Lyden notes. “We expect that as endovascular techniques continue to evolve, we can feel even more confident in this conclusion.”
“Evaluating the best option for restoring blood flow in patients with narrowing of the aorta and iliac arteries can be challenging,” observes Scott J. Cameron, MD, PhD, Section Head of Vascular Medicine at Cleveland Clinic, who was not involved in the study. “This retrospective analysis by our vascular surgery group showed that, in medically complex patients with similar vascular anatomy, the less invasive procedure of endovascular aortoiliac reconstruction is an alternative to open surgical bypass in a center of excellence for vascular care, offering a shorter hospital stay, less blood loss and fewer wound complications. Future studies will focus on confirming this observation in a larger cohort of patients and evaluating quality-of-life and walking symptoms in patients undergoing either procedure.”
Advertisement
Advertisement
Initial data indicate tolerability and promising cardiac remodeling effects
LLM-driven system uses both structured and unstructured data, provides auditable justifications
A new CME opportunity in Chicago, May 15-16
After four decades, refinements to the gold standard of bypass continue as new insights emerge
Why definitive surgical closure is the gold standard, and new ways to make it possible
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Cleveland Clinic’s new dedicated program offers nuanced care for a newly recognized cardiovascular risk factor
Scenarios where experience-based management nuance can matter most