Weakened endorsements in settings of normal EF and mild-moderate LV dysfunction may cause harm
When clinical practice guidelines are issued, attention to the underlying data and accurate characterization of evidence matter. That’s the message Cleveland Clinic cardiothoracic surgeon Faisal Bakaeen, MD, is advancing in the wake of the contentious 2021 American College of Cardiology (ACC)/American Heart Association (AHA)/Society for Cardiovascular Angiography & Intervention (SCAI) guidelines on coronary artery revascularization published online in December 2021 (J Am Coll Cardiol. 2022;79[2]:e21-e129).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In a presentation at the AHA’s 2022 scientific sessions in November and in a recent editorial in JAMA Surgery, Dr. Bakaeen argued that the guidelines’ downgrade of coronary artery bypass graft surgery (CABG) relative to medical therapy in patients with ischemic heart disease and severe three-vessel disease is unjustified and not based on assessment of all evidence to date.
In his editorial, he and his two co-authors contend that the incident has implications beyond the use of CABG. “It underscores the importance of attention to source documents instead of blind acceptance of summary evidence,” they write.
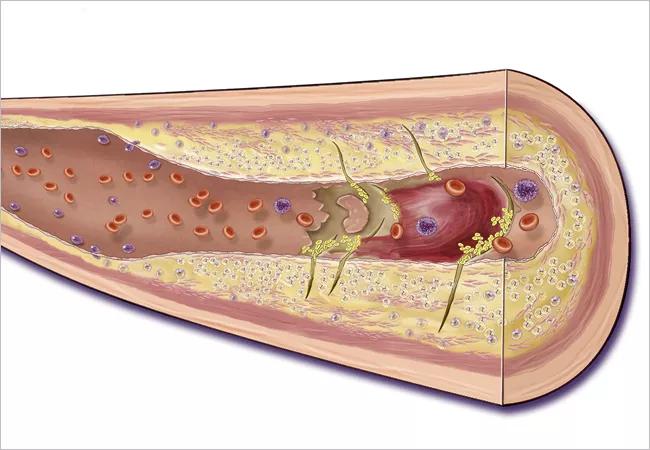
The controversy surrounding the 2021 ACC/AHA/SCAI guidelines centers on two specific changes in recommendations they introduced, both in patients with stable ischemic disease and severe three-vessel disease and with survival as the endpoint:
Soon after the guidelines were issued, they prompted rebuttal editorials from the Society of Thoracic Surgeons and the American Association for Thoracic Surgery as well as numerous other professional cardiovascular societies, some with significant cardiologist membership. The guideline authors defended the recommendations as data-based and dismissed the objections as stemming from differences in the interpretation of evidence, but Dr. Bakaeen disagrees. “Current evidence does not support the blanket downgrading of CABG for these patient populations with three-vessel disease,” he says.
Advertisement
“This controversy reflects the absence of strong contemporary evidence from prospective randomized trials comparing outcomes for CABG versus medical therapy, whereas population-based studies continue to show the benefit of CABG, apart from clinical experience showing improved outcomes of individual patients,” says Steven Nissen, MD, Chief Academic Officer of Cleveland Clinic’s Heart, Vascular & Thoracic Institute. “Nevertheless, medical therapy has improved substantially in the decades following the randomized controlled clinical trials that established the superior benefits for CABG. We need new high-quality evidence to resolve this controversy in low-risk patients in whom the benefits of CABG versus medical therapy are unclear.”
In his editorial, Dr. Bakaeen and his co-authors note that the new guidelines present no new evidence directly comparing CABG with medical therapy to support the downgrading of CABG. They also point out the following:
Advertisement
“The guidelines’ evidence base inadequately incorporated the typical patient population that undergoes CABG nowadays,” Dr. Bakaeen observes. “The guidelines extrapolate findings from lower-risk populations with low adverse cardiovascular event rates, and these data are further limited by short-term follow-up. When we offer CABG, we are talking about a lifelong therapy for patients at significant risk for adverse events at baseline.”
He notes that a recent Society of Thoracic Surgeons database publication shows that a contemporary CABG population constitutes patients who are two to four times more likely to have peripheral or cerebrovascular disease or heart failure than patients in the ISCHEMIA study. “Only 36 % of patients in ISCHEMIA had significant proximal left anterior descending lesions,” Dr. Bakaeen says. “Despite this, the ISCHEMIA study was inappropriately considered by the 2021 guidelines as the primary evidence for downgrading CABG. In addition, errors and inconsistencies were identified in ISCHEMIA publications that led to two separate published corrections. Recently, the only surgeon serving on the ISCHEMIA steering committee resigned amid concerns about data accuracy.”
He adds that while it is well established that medical therapy is cornerstone initial management for patients who may ultimately be candidates for coronary revascularization, “the relevant evidence is strong regarding the efficacy of CABG over medical therapy in prolonging survival for patients with multivessel disease regardless of ejection fraction.” He notes that this is supported by a recent meta-analysis of individual patient data from randomized trials (J Thorac Cardiovasc Surg. Epub 9 June 2022).
Advertisement
“We must keep in mind the cost of a baseless downgrade of CABG in this setting,” Dr. Bakaeen continues. “Death and adverse events are well documented in patients on waiting lists for CABG. When CABG is deferred, it is more likely to be performed nonelectively or when the ejection fraction is low, and both of these scenarios are associated with increased perioperative morbidity and mortality.”
“There are no new persuasive data to justify this downgrade,” says Stephen Ellis, MD, Director of Interventional Cardiology and Senior Academic Officer of Cleveland Clinic’s Heart, Vascular & Thoracic Institute, in response to an invitation to comment. “That said, the data supporting the survival benefit of CABG come from studies that are now two to three decades old, and both surgical and medical treatments have evolved a lot since then. Importantly, too, we often refer patients for CABG to treat their symptoms without an expectation of survival benefit. This is wholly justified and supported in the guidelines, with a Class I recommendation.”
Dr. Bakaeen notes that at Cleveland Clinic, each patient is treated based on the complexity and severity of his or her coronary disease, along with any other health conditions and the degree of frailty. “We tailor the treatment choice to the specific findings and the patient’s preferences and priorities,” he says. “Quality and durable outcomes are the goal.”
Advertisement
Advertisement

Pediatric specialists unpack new evidence, considerations for care and what’s ahead
27th offering of this CME favorite to be held March 6-9 in Hollywood, Florida

Metabolites from animal product substrates implicated in heart failure development in community cohorts

ACC committee underscores need to properly weigh benefits in risk-benefit calculations

BITA grafts themselves are rarely to blame, and outcomes can be good

Two cardiac surgeons explain Cleveland Clinic’s philosophy of maximizing arterial graft use

A reliable and reproducible alternative to conventional reimplantation and coronary unroofing

Cleveland Clinic-pioneered repair technique restores a 61-year-old to energetic activity