Series finds short-term outcomes excellent, but BAV may be less durable
Early results for aortic root replacement with bicuspid aortic valve (BAV) reimplantation are similar to those with the better-established tricuspid aortic valve (TAV) reimplantation. However, outcomes between the two procedures diverge over time, indicating that long-term surveillance is needed for patients with a BAV reimplantation — and raising concern over its routine use.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
So conclude Cleveland Clinic investigators in their report of a retrospective case series published in the Journal of Thoracic and Cardiovascular Surgery (JTCVS) (2022;163[1]:51-63.e5).
“Our experience indicates that valve-preserving aortic root replacement for aortic aneurysm can be an attractive option for appropriate patients with either a tricuspid or a bicuspid aortic valve,” says senior author Lars Svensson, MD, PhD, Chair of Cleveland Clinic’s Heart, Vascular & Thoracic Institute. “But caution is needed with BAV reimplantation, to ensure careful selection of appropriate patients with bicuspid valves.”
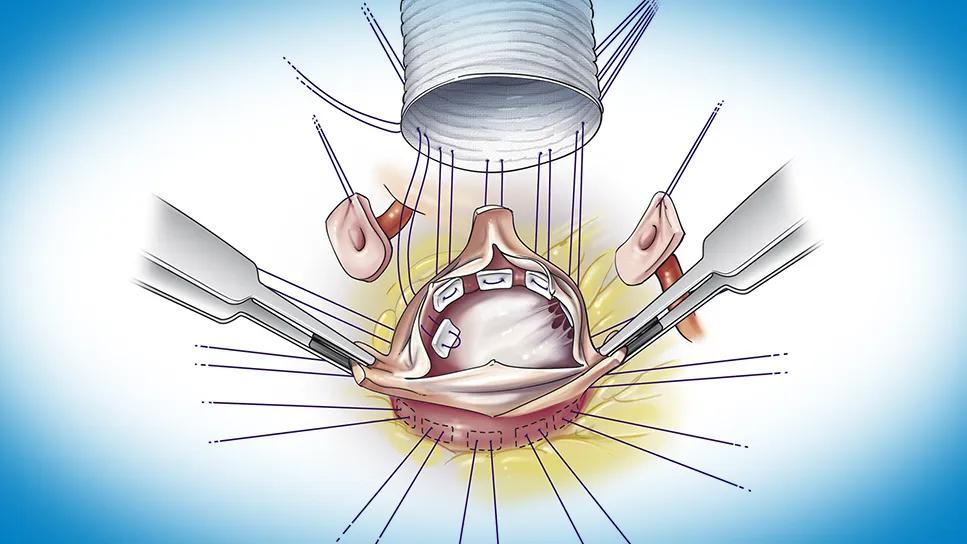
Patients with aortic root dilatation — with or without dissection — are traditionally treated with a Bentall operation, which involves replacing the damaged portion of the aorta as well as the aortic valve with a biologic or mechanical prosthesis. But if the native valve is in good condition, Cleveland Clinic surgeons prefer reimplantation over replacement based on the world’s largest experience with reimplantation operations — over 1,200 to date. Evidence indicates that reimplantation lowers the risk of thromboembolic and bleeding complications, particularly in patients with connective tissue disease. It also may enhance aortic anulus stabilization, helping prevent further dilatation and aortic regurgitation — as well as a later surgery.
Although good evidence exists for excellent outcomes of valve reimplantation for patients with a TAV — e.g., 95% or better freedom from reoperation at 10 years — less is known about results with a BAV.
Advertisement
Patients who underwent aortic root replacement with aortic valve reimplantation at Cleveland Clinic between January 2002 and July 2017 were included in the study. The cohort consisted of 607 adults, of whom 92 had a BAV reimplantation and 515 had a TAV reimplantation. To facilitate comparability of the two groups, 71 matched pairs were created using 28 preoperative variables.
Median follow-up of the BAV group was 2.8 years, with 25% followed for more than 4.7 years and 10% for more than 6.6 years.
In-hospital morbidity and mortality were very low and similar between the two groups, including one death (in the BAV group), one stroke (in the TAV group) and renal failure requiring dialysis in one patient in each group. The need for blood transfusion was similar between the groups.
At five years, survival rates were high and similar (100% in the BAV group, 95% in the TAV group, P = 0.07). However, concerning trends emerged in the BAV cohort (relative to the TAV cohort) over time, including the following:
According to Dr. Svensson, the jury is still out on how valve reimplantation stacks up against other alternatives, such as a root remodeling operation, for a given patient with a BAV. He points out that determining the best aortic valve option is especially important for young patients. While some argue that at least offering them a good option for 10 or 15 years is reasonable, this approach makes it more likely the patient will need another operation when older and likely at higher risk.
Advertisement
“Longer-term follow-up and meta-analysis of data from multiple institutions are needed to determine whether BAV reimplantation measures up to the traditional Bentall operation with a mechanical or biological valve,” he advises.
The article describes technical considerations that, in the experience of Cleveland Clinic surgeons, contribute to the success of a durable BAV or TAV reimplantation procedure. In brief, they recommend special attention to the following, known as the CLASS schema:
“Reimplantation procedures have been well received by patients at the time of surgical intervention on the aorta,” observes study co-author Brian Griffin, MD, Section Head of Cardiovascular Imaging at Cleveland Clinic. “It’s not surprising that BAV reimplantation would have a less optimal long-term outcome than TAV reimplantation, given the inherent abnormality of the bicuspid valve. Notwithstanding the higher complication rate described in our study, BAV reimplantation has a role in management of individual patients, especially those who wish to avoid mechanical valve replacement and the need for long-term anticoagulation.”
Advertisement
Yet BAV reimplantation is an option best deployed by experienced centers and in well-selected patients. “In view of this study’s results and the fact that reimplantation is so technically demanding and requires more surgeon expertise,” Dr. Svensson concludes, “mechanical valves may be the best option for younger patients undergoing root surgery and at centers that lack expertise with reimplantation operations.”
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more