One-time infusion of adenovirus-based therapy is designed to restore heart muscle function

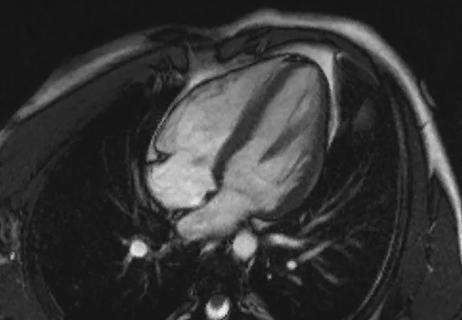
Human clinical testing of TN-201, an experimental gene therapy for hypertrophic cardiomyopathy (HCM) associated with myosin binding protein C3 gene (MYBPC3) mutation, has begun with infusion of the therapy in the first patient in a phase 1b trial at Cleveland Clinic in early October.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The goal of treatment with TN-201, a first-in-class adenovirus-based therapy, is to deliver a working copy of the MYBPC3 gene to the heart muscle in hopes of halting disease progression. In preclinical studies, a one-time intravenous infusion of the therapy restored normal levels of myosin binding protein C3, which regulates contraction of heart muscle, reversing HCM.
“The therapy is administered as a single injection to stimulate protein formation with the aim of achieving normal myocardial function,” says study investigator Milind Desai, MD, MBA, Director of Cleveland Clinic’s Hypertrophic Cardiomyopathy Center and Vice Chair of its Heart, Vascular & Thoracic Institute. “If it is ultimately shown to be safe and effective in humans, it could prove to be a one-time solution for a fairly common form of HCM.”
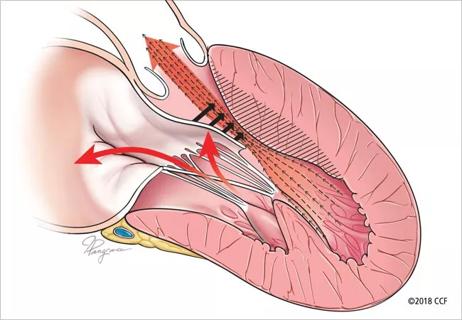
HCM, the leading cause of sudden cardiac death before age 30, commonly has a genetic etiology. The most frequent genetic cause is MYBPC3 mutation, accounting for an estimated 20% of all HCM cases.
“This mutation essentially results in a protein deficiency state,” Dr. Desai explains. “People with a defective MYBPC3 gene produce only 60% to 70% of the amount of myosin-binding protein C3 needed for heart function. Patients who have MYBPC3-associated HCM are at heightened risk for accelerated decline and serious disease complications.”
The newly launched trial of TN-201 is an open-label investigation among patients diagnosed with MYBPC3-associated nonobstructive HCM who are symptomatic and have an implantable cardioverter defibrillator.
Advertisement
Investigators are initially targeting an enrollment of six adults in the multicenter trial, which could eventually increase to as many as 15. All patients will receive the therapy as a two- to three-hour infusion, be monitored on an inpatient basis for a week, and then be followed for five years for treatment response.
Primary outcome measures are safety and tolerability over five-year follow-up. The secondary outcome measure is change in quality of life, as assessed by the Kansas City Cardiomyopathy Questionnaire Clinical Summary Score, at week 52 after TN-201 infusion.
Additionally, patients will undergo heart biopsies at post-infusion weeks 8 and 52 to assess expression levels of vector genomes and transgene messenger RNA and MYBPC3 protein in the right ventricular septum. Changes in N-terminal pro BNP and high-sensitivity cardiac troponin I levels also will be assessed over five years, as will changes in echocardiography measures, peak exercise capacity and New York Heart Association functional class.
The initial dosage of the infusion is 3E13 vg/kg, which was associated with near-maximal efficacy in preclinical studies. Plans for dose escalation to 6E13 vg/kg, as needed, and/or enrollment of additional patients in the initial cohort, will be informed by an independent safety review following the initial cohort.
“As per protocol, we treated the first patient in the trial, a 27-year-old woman, earlier this month,” Dr. Desai notes. “She was monitored in the hospital for a week before being discharged and is doing well so far.”
Advertisement
Results are expected in 2024. If TN-201 is found to be safe and effective, a phase 2 trial will be launched in a larger population.
Currently only one disease-specific medication, mavacamten, is available to treat HCM. Approved for commercial use in 2022, in part based on a trial led by Cleveland Clinic, it is indicated for treatment of obstructive HCM to reduce the need for invasive procedures. Surgical options include septal myectomy and alcohol ablation, but few high-volume centers perform these procedures, which may limit patient access and require repeat intervention.
“Our understanding of HCM has progressed to the point where we are developing novel medical treatments that will, hopefully, avoid the need for septal reduction therapy,” says Dr. Desai. “Right now, we are focused on determining whether the impressive results seen in preclinical studies of TN-201 can be translated into a safe and efficacious treatment for patients.”
Disclosure: Dr. Desai is a paid consultant to Tenaya Therapeutics, which is sponsoring the study reported here.
Image at top: A research nurse coordinator readies the infusion of TN-201 for the first patient in the trial.
Advertisement
Advertisement

End-of-treatment VALOR-HCM analyses reassure on use in women, suggest disease-modifying potential

Cardiac imaging substudy is the latest paper originating from the VANISH trial

Vigilance for symptom emergence matters, a large 20-year analysis reveals

Phase 3 ODYSSEY-HCM trial of mavacamten leaves lingering questions about potential broader use

5% of flagged ECGs in real-world study were from patients with previously undiagnosed HCM

High composite score in myectomy specimens signals worse prognosis
Few patients report left ventricular dysfunction or heart failure after one year
Avoidance of septal reduction therapy continues while LVEF dysfunction remains infrequent