Scenarios where experience-based management nuance can matter most
Of the 1,000-plus mitral valve surgeries performed at Cleveland Clinic each year, well over half are mitral valve repairs, either isolated or in combination with other heart surgeries. Roughly 10% to 20% of those repairs each year involve repair of Barlow’s valve (i.e., bileaflet prolapse).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
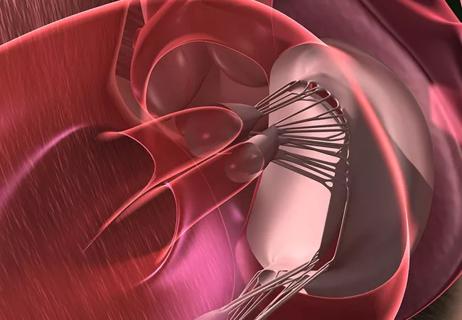
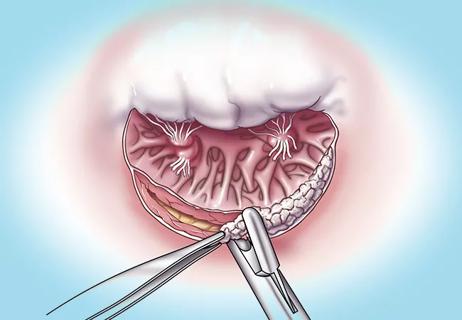
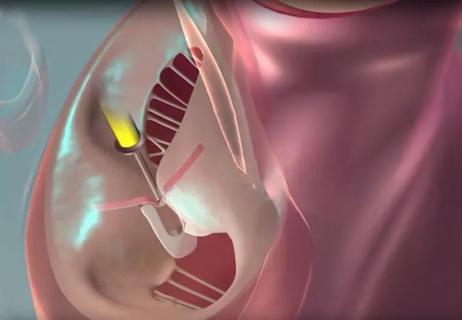
Barlow’s valve is a form of degenerative mitral valve disease characterized by large valve size with redundant and myxomatous tissue on both leaflets, causing the valve to appear thick and swollen. Conventional repair techniques for fibroelastic deficiency are typically inadequate in this setting. Cleveland Clinic surgeons employ a technique that avoids extensive cutting and suturing in favor of treating the chordae instead of the leaflets. Using PTFE sutures, they create artificial chordae of varying lengths for the anterior and posterior leaflets, allowing the coaptation zone to be adjusted for precise repair and closure. In cases of isolated repair, the procedure often can be done with robotic assistance, which reduces cross-clamp time relative to open surgery.
Outcomes of Barlow’s valve repair at Cleveland Clinic are consistent with those for isolated mitral valve repair overall — operative mortality well below 0.1% and zero or mild residual mitral regurgitation (MR) in over 99% of cases.
Just as Barlow’s valve can require nuanced surgical management, it also demands special vigilance during evaluation.
“Characteristic echocardiographic features are excess tissue and long leaflet length,” says Milind Desai, MD, MBA, a cardiovascular imaging expert with Cleveland Clinic’s Mitral and Tricuspid Valve Center. “Often the regurgitation in these patients is moderate rather than severe. It frequently is late-peaking, not encompassing the full systolic part of the cardiac cycle. For this reason, use of instantaneous PISA [proximal isovelocity surface area] may overestimate the degree of MR severity. So for patients with bileaflet prolapse, it’s important to quantify regurgitant fraction and regurgitant volume to ascertain the leak severity. Once MR is properly quantified to be in the severe range, the patient should be referred for valve repair.”
Advertisement
In the setting of Barlow’s valve, he adds, vigilance is needed for malignant mitral valve prolapse, a rare subset of mitral prolapse that carries a high risk of life-threatening arrhythmias and sudden cardiac death (SCD), frequently in young women, even in the absence of significant MR. Malignant mitral valve prolapse has been reported in 1.2% to 8.0% of SCD cases.
“Identifying malignant mitral valve prolapse can be like finding a needle in a haystack, but it’s imperative in patients with bileaflet prolapse because the stakes are so high,” Dr. Desai notes. The condition is associated with mitral annular disjunction on echocardiography, as well as with specific ECG changes, fibrosis in papillary muscles and an arrhythmogenic substrate. “It’s essential to look for arrhythmias, take a detailed history, including family history, and make sure there’s no history of palpitations. If echo shows mitral annular disjunction and Barlow’s valve is suspected, cardiac MRI should be considered to detect and evaluate fibrosis and any resulting arrhythmogenic phenotype. Referral to an electrophysiologist may be needed for a potential defibrillator.”
Some cases of Barlow’s valve are part of a broader clinical entity known as Barlow’s syndrome, which can be hereditary, linked to genetic conditions like Marfan syndrome or other connective tissue disorders. In Barlow’s syndrome, the aforementioned characteristics of a large mitral valve with bileaflet prolapse and excessive myxomatous tissue are often accompanied by non-ejection systolic clicks on auscultation, palpitations, arrhythmias arising from fibrosis, chest pain and sometimes an asthenic habitus. Barlow’s syndrome is associated with occasional cases of SCD, consistent with malignant mitral valve prolapse.
Advertisement
Given the broad spectrum of clinical effects of Barlow’s syndrome, patients with the syndrome treated at Cleveland Clinic often undergo combined operations to repair the mitral valve in addition to another needed heart procedure.
“The spectrum of mitral valve repairs we do for Barlow’s syndrome can be quite wide,” says Lars Svensson, MD, PhD, Chief of Cleveland Clinic’s Heart, Vascular and Thoracic Institute, who often repairs Barlow’s valve in combination with aortic valve operations, frequently in patients with Marfan syndrome (see Figure). “In these patients, if the MR is moderate, often all that’s needed is to put in a ring to support the mitral valve. If it’s more severe, we need to use artificial chordae and resect some of the posterior leaflet to reduce its size. That also serves to reduce the risk of systolic anterior motion.”

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c9b17569-f898-467e-bfa1-07ebdfbbfa5e/25-HVI-6845758-CQD-inset)
Figure. Photos from surgery in a young woman who presented with severe heart failure and poor pulmonary function tests. She was found to have Marfan syndrome with a wide-open Barlow’s valve measuring 6 cm as well as severe tricuspid valve regurgitation and aortic valve regurgitation with an aortic root aneurysm. The mitral valve, tricuspid valve and aortic valve were successfully repaired in conjunction with aortic root reimplantation. She was discharged without need for lifelong warfarin therapy.
He adds that while some operators have reported using the Alfieri stitch or a mitral transcatheter edge-to-edge repair (M-TEER) clip in this setting, the durability of these approaches is questionable. “Because the tissue is myxomatous and fragile, it generally requires a proper repair,” Dr. Svensson explains.
One uncertainty is whether repairing Barlow’s valve will cure arrhythmias that are related to scar tissue arising from the Barlow’s valve. “In recent years I have repaired Barlow’s valve in several patients to treat severe arrhythmias in the absence of severe MR,” Dr. Svensson notes. “Those patients’ arrhythmias were resolved, but there are no large trials showing definitive benefit specifically for arrhythmias in this setting because patient numbers are too small.”
Advertisement
Of course, the presence of MR itself significantly raises the risk of arrhythmias, especially atrial fibrillation (AF), even outside the context of Barlow’s valve or Barlow’s syndrome.
“Any patient with a history of atrial fibrillation who is undergoing mitral valve repair should receive a maze procedure along with a clip or occlusion of the left atrial appendage at the time of their valve repair,” Dr. Svensson says. “We do a lot of maze procedures in combination with mitral valve repairs every year — and in combination with mitral valve replacement when replacement is necessary. It adds a little time to the surgery, but by getting the patient back into normal heart rhythm, it raises the prospect of curing two problems with one operation.”
Cleveland Clinic surgeons generally use a biatrial approach to surgical ablation rather than a left-atrium-only approach. The need for surgical ablation of AF typically excludes robotically assisted mitral valve repair, although many cases combining mitral valve repair with the maze procedure can be done with a minimally invasive J incision.
Whenever possible, Cleveland Clinic electrophysiologists are involved in the preoperative evaluation of patients undergoing a maze procedure with mitral valve repair, to help ensure comprehensive arrhythmia care. They also may be involved after surgery if patients need a postoperative pacemaker or have recurrent arrhythmias.
“Postoperatively, some patients may have conduction problems or sinus node dysfunction that may require a pacemaker,” says Oussama Wazni, MD, MBA, Section Head of Cardiac Electrophysiology and Pacing.
Advertisement
“Also, occasional patients have AF recurrence or end up with atrial flutter after a maze procedure,” Dr. Wazni continues. “Our electrophysiologists are experts in treating post-maze arrhythmias with catheter-based mapping and ablation. This includes post-maze atrial flutter, which can be challenging to map. We increasingly offer pulsed field ablation for post-maze AF and flutter, as it delivers faster and safer ablation compared with thermal methods.”
Another scenario where electrophysiologists loom large is when candidates for mitral valve repair have ventricular tachycardia or premature ventricular contractions. Dr. Wazni notes that optimal management in these infrequent cases is complicated and not well defined, even for a center like Cleveland Clinic with pioneering expertise in ablation — including pulsed field ablation — of ventricular arrhythmias.
“Scientific understanding of these cases is still evolving,” he says. “Often these patients require a cardiac MRI to assess the degree of scar tissue or disjunction involved. There currently is no guidance, so volume-based expertise is helpful. We cannot promise definitive answers in these complex cases, but we will bring to bear thoughtful judgment and comprehensive multidisciplinary assessment grounded in our large experience base.”
Advertisement

Optimal management requires an experienced center

Multimodal evaluations reveal more anatomic details to inform treatment

Provides option for patients previously deemed anatomically unsuitable
While mortality was unaffected, later surgery was associated with more reoperations
Surgical tips on debridement of calcification to optimize valve replacement
Superiority continues even after significant crossovers from control group at 2 years

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon