Distinct MRI signature includes lesions beyond the corpus callosum, features predictive of vision and hearing loss
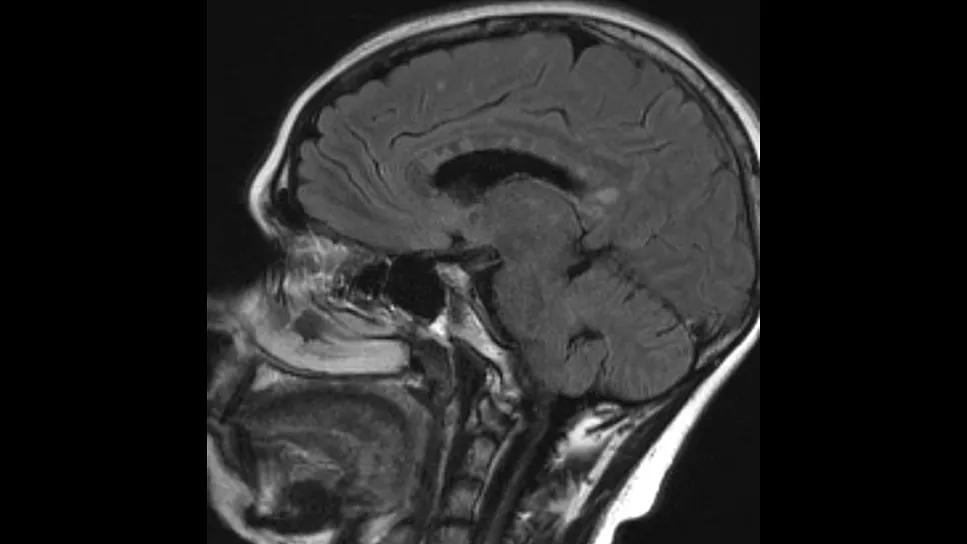
Cerebrovascular involvement and deep brain lesions are prominent and underrecognized MRI features of Susac syndrome (SuS) and correlate with vision and hearing loss in those affected.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Those are among key findings of two studies presented at the International Stroke Conference 2026 that were derived from Cleveland Clinic’s Susac Syndrome Retrospective Cohort, the largest such single-center cohort reported to date.
“Our findings broaden the imaging spectrum of Susac syndrome and suggest that small-vessel infarcts in these patients may predict retinal vasculitis and hearing loss,” says G. Abbas Kharal, MD, a vascular neurologist and neuroimmunologist in Cleveland Clinic’s Cerebrovascular Center and leading investigator of both studies. “The imaging markers we identified may help identify patients at risk for severe disease and help guide immunotherapy.”
SuS and primary angiitis of the central nervous system (PACNS) are rare, autoimmune, small-vessel vasculitides that share imaging and clinical features. Accurately differentiating between them is critical because management of the two conditions differs substantially.
SuS involves the central nervous system (CNS), retina and cochlea. Clinical symptoms include unilateral or bilateral visual field defects, sensorineural hearing loss, headache, confusion and memory impairment. The hallmark cerebrovascular findings on brain MRI in patients with SuS include corpus collosum lesions that resemble snowballs, but imaging can also show small-vessel infarcts in other areas of the brain similar to the small-vessel subtype of PACNS.
PACNS, in contrast, is confined to the CNS, and vessel inflammation and destruction lead to progressive, debilitating neurological deficits along with headaches, seizures and memory issues. Neuroimaging is always abnormal. Ischemic infarctions — often multiple and bilateral — are the most common lesions.
Advertisement
“The triad of encephalopathy and vision and hearing loss with SuS is well known, but cerebrovascular involvement has not been well defined,” says Dr. Kharal. “Our aim was to systematically characterize the features of SuS and identify its imaging hallmarks.”
Seventy patients from the Susac Syndrome Retrospective Cohort were included in the first study. Using charts, the authors reviewed clinical data about neurological, ophthalmologic and audiologic evaluations. They also examined brain MRI with and without contrast, fluorescein angiography, optical coherence tomography and audiography in greater depth.
Descriptive statistics were used to summarize clinical and imaging features of the cohort, with medians for continuous variables and frequencies for categorical variables.
Three-quarters of the SuS patients were female. The cohort had a median age of 34 years. The most common clinical symptom at presentation was vision loss, seen in 89.6%, followed by hearing loss (82.9%), cognitive impairment (76.8%) and confusion (69.1%).
MRIs were available for 57 patients, of which 48 (84%) revealed corpus callosum lesions. Cerebellar, brainstem and middle cerebellar peduncle involvement was seen in 47.4%, 24.6% and 15.8% of the scans, respectively. Deep gray matter lesions were noted on 35.1% of MRIs and leptomeningeal enhancement on 19.3%. Over half the scans (52.6%) showed small-vessel infarcts, nearly all of which (96.7%) were deep subcortical.
Non-CNS manifestations of SuS included branch retinal artery occlusions (BRAOs) in 75.9% of patients, 59.1% of which were bilateral. A statistically significant association was found between cerebrovascular small-vessel infarcts and new BRAOs regardless of acuity or depth.
Advertisement
Ophthalmologic evaluations showed that 62.3% of SuS patients had vascular leakage and 41.2% had retinal atrophy. Nearly three-quarters (71.4%) had sensorineural hearing loss on audiography.
“Our data suggest that as many as 70% of SuS patients may have the complete triad of symptoms, in contrast to the 40% previously reported in the literature,” says Dr. Kharal. “Half the cohort had tiny infarcts associated with BRAO, which can lead to blindness and have implications for treatment.”
Sixty-three patients from the SuS cohort and 33 patients treated for PACNS at Cleveland Clinic’s Cerebral Vasculitis Clinic from 2015 to 2024 were included in the second study. All the PACNS patients had small-vessel disease and were seen for biopsy- or angiography-supported diagnosis and exclusion of systemic vasculitis.
The researchers compared features of SuS and PACNS on brain MRI to identify distinguishing imaging markers in patients with CNS-predominant presentations. Scans were reviewed for corpus callosum involvement, white matter enhancement, infarct patterns, cerebellar lesions, leptomeningeal enhancement and gray matter involvement.
Corpus callosum lesions were present on 83.6% of scans from SuS patients versus 19.4% of those from PACNS patients (P < .001). Cerebellar involvement also was more common with SuS (45.9% vs. 19.4; P = .013). In contrast, enhancing white matter lesions and lacunar infarcts were more common with PACNS (65.5% vs. 27.3% [P = .001] and 29.0% vs. 11.5% [P = .045], respectively). Nearly all patients in the two groups had periventricular/subcortical white matter involvement.
Advertisement
According to Dr. Kharal, the studies yield the following take-home messages:
“These are the largest studies to characterize the imaging spectrum of Susac syndrome and to compare it with PACNS in such a sizable cohort,” concludes Dr. Kharal. “Further research is underway to determine whether acute cerebrovascular manifestations correlate with disease severity and relapse risk.”
He adds that the reported research was made possible by the dedication of all co-authors and team members, including Adam Brown, MD; Sedat Gul, MD; Casandra MacLeod, DO; Gowtham Yerneni, MD candidate; and Nicolas Thompson, MS.
Advertisement
Advertisement

Despite less overall volume loss than in MS and NMOSD, volumetric changes correlate with functional decline

It’s time to get familiar with this emerging demyelinating disorder

From dryness to diagnosis
Early experience with the agents confirms findings from clinical trials

Despite advancements, care for this rare autoimmune disease is too complex to go it alone
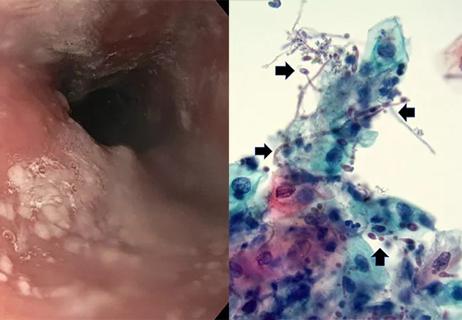
Treatment for scleroderma can sometimes cause esophageal symptoms
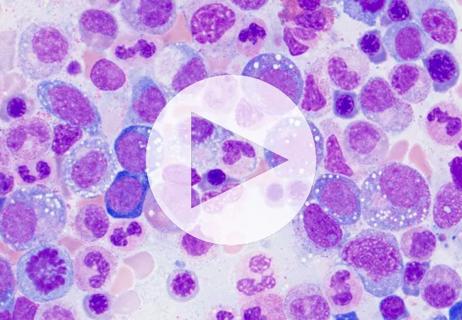
Patient’s symptoms included periorbital edema, fevers, weight loss

Could the virus have caused the condition or triggered previously undiagnosed disease?